Coloanal Pull Through
Coloanal Pull Through is a complex surgical procedure designed to treat specific conditions affecting the rectum and lower colon, often involving the removal of diseased tissue while preserving anal function. This approach aims to restore bowel continuity and improve the quality of life for patients facing challenging colorectal health issues.
Key Takeaways
- Coloanal Pull Through is a surgical technique to remove diseased rectum/colon and connect the remaining colon directly to the anus.
- It is primarily performed for conditions like rectal cancer, inflammatory bowel disease, or familial adenomatous polyposis.
- The procedure involves several stages, including tissue removal, colon mobilization, and anastomosis.
- Recovery requires careful post-operative management, focusing on pain control, diet, and managing potential bowel function changes.
- Long-term follow-up is crucial to monitor healing and address any complications or functional adjustments.
What is Coloanal Pull Through?
Coloanal Pull Through is a surgical procedure that involves the removal of a diseased segment of the rectum, and sometimes a portion of the lower colon, followed by the direct connection of the remaining healthy colon to the anus. This technique is primarily employed to treat conditions such as low rectal cancer, severe inflammatory bowel disease affecting the rectum, or familial adenomatous polyposis, where a significant part of the rectum needs to be resected. The goal is to eradicate the disease while preserving the patient’s natural anal sphincter function, thereby avoiding a permanent colostomy whenever possible.
The procedure is considered a significant advancement in colorectal surgery, offering patients the potential for a better quality of life compared to older techniques that often necessitated a permanent stoma. It requires meticulous surgical skill and careful patient selection to optimize outcomes and minimize complications. According to the American Cancer Society, colorectal cancer is the third most common cancer diagnosed in both men and women in the United States, highlighting the importance of effective surgical interventions like the Coloanal Pull Through for appropriate cases.
The Coloanal Pull Through Procedure Explained
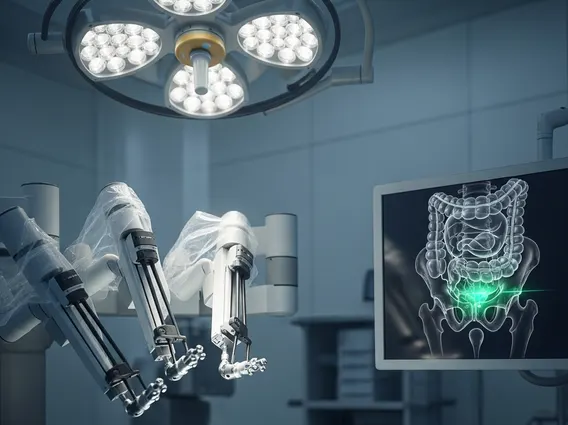
The Coloanal Pull Through procedure is a multi-stage operation that can be performed using open, laparoscopic, or robotic surgical techniques, depending on the patient’s condition and the surgeon’s expertise. The primary objective is to remove the diseased section of the rectum and then “pull through” the healthy colon to create a new connection to the anal canal, known as a coloanal anastomosis. This intricate process ensures the restoration of bowel continuity.
The steps involved in a Coloanal Pull Through surgery explained typically include:
- Resection: The diseased portion of the rectum and any affected surrounding tissues are carefully removed.
- Colon Mobilization: The remaining healthy colon is freed from its attachments and mobilized sufficiently to reach the anus without tension.
- Anastomosis: The mobilized colon is then pulled down through the pelvic cavity and connected directly to the anal canal, just above the anal sphincter muscles. This connection, or anastomosis, is critical for maintaining continence.
- Temporary Diversion (Optional): In many cases, a temporary diverting ileostomy or colostomy is created higher up in the abdomen. This allows the newly created coloanal anastomosis to heal without the passage of stool, reducing the risk of complications like anastomotic leak. This temporary stoma is usually reversed in a subsequent surgery after several weeks or months.
The choice of surgical approach and whether a temporary stoma is needed is determined by the surgeon based on factors such as the extent of the disease, the patient’s overall health, and the quality of the tissues involved.
Coloanal Pull Through Recovery and Post-Operative Care
Coloanal Pull Through recovery is a gradual process that requires careful management both in the hospital and at home. Immediately after surgery, patients typically spend several days to a week in the hospital, where pain management, fluid balance, and early mobilization are prioritized. Diet is gradually advanced from clear liquids to solids as bowel function returns. Patients with a temporary stoma will receive education on stoma care before discharge.
Upon returning home, patients can expect significant changes in bowel habits. It is common to experience increased stool frequency, urgency, and sometimes difficulty with continence in the initial weeks and months following surgery. These symptoms often improve over time as the body adapts and the neorectum (the newly formed colon segment) stretches and gains capacity. Dietary modifications, such as avoiding trigger foods and increasing fiber, can help manage these symptoms. Pelvic floor exercises may also be recommended to strengthen the anal sphincter muscles.
Long-term follow-up with the surgical team is essential to monitor healing, address any persistent issues, and manage potential complications such as anastomotic stricture (narrowing of the connection) or chronic pouchitis (inflammation of the neorectum). For patients who had a temporary stoma, the reversal surgery is typically scheduled once the coloanal anastomosis has fully healed, usually 2-3 months post-initial operation. Full recovery, including adaptation to new bowel function, can take several months to a year.