Colitis
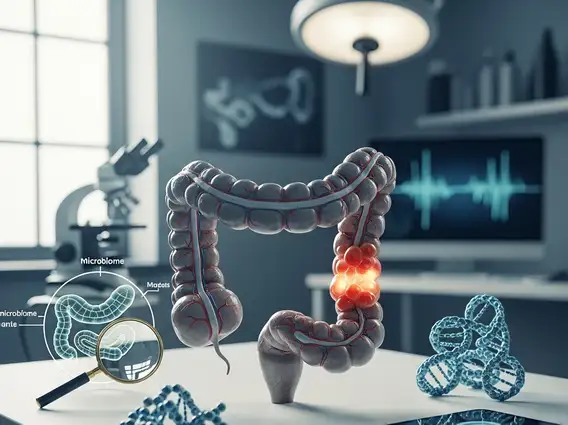
Colitis is a medical condition characterized by inflammation of the colon, the largest part of the large intestine. This inflammation can lead to a range of uncomfortable symptoms and, if left untreated, may result in serious complications.
Key Takeaways
- Colitis is inflammation of the colon, presenting with symptoms like abdominal pain and diarrhea.
- It can stem from various causes, including infections, autoimmune responses, and reduced blood flow.
- Diagnosis typically involves endoscopic procedures and imaging, guiding appropriate treatment.
- Treatment options range from medication to surgery, depending on the underlying cause and severity.
- Managing colitis at home involves dietary adjustments, stress reduction, and adherence to medical advice.
What is Colitis? Symptoms, Causes, and Types Explained
Colitis refers to the inflammation of the inner lining of the colon. This condition can manifest in various forms, each with distinct characteristics and underlying mechanisms. Understanding colitis and its symptoms is crucial for early detection and management, as symptoms often include abdominal pain, cramping, and changes in bowel habits.
Common symptoms associated with colitis can vary in intensity and may include:
- Abdominal pain and cramping
- Persistent diarrhea, which may contain blood or pus
- Urgent need to have a bowel movement
- Weight loss
- Fatigue
- Fever
- Dehydration
The causes and types of colitis explained are diverse. Some common types include:
- Ulcerative Colitis: A chronic inflammatory bowel disease (IBD) causing long-lasting inflammation and ulcers in the innermost lining of the large intestine and rectum.
- Crohn’s Colitis: A form of Crohn’s disease that specifically affects the colon, characterized by inflammation that can penetrate deeper layers of the bowel wall.
- Ischemic Colitis: Occurs when blood flow to a section of the colon is reduced, often due to narrowed or blocked arteries, leading to inflammation and tissue damage.
- Infectious Colitis: Caused by bacteria, viruses, or parasites, often leading to acute inflammation and symptoms like severe diarrhea.
- Microscopic Colitis: Characterized by inflammation only visible under a microscope, with two main subtypes: collagenous colitis and lymphocytic colitis.
- Allergic Colitis: More common in infants, often triggered by certain proteins in formula or breast milk.
The specific cause dictates the approach to treatment and management, highlighting the importance of accurate diagnosis.
Colitis Diagnosis and Treatment Options
Accurate colitis diagnosis and treatment options are essential for managing the condition effectively. Diagnosis typically begins with a thorough medical history and physical examination. Further diagnostic tests may include stool samples to check for infection, blood tests to look for inflammation markers or anemia, and imaging studies such as CT scans or MRI to visualize the colon.
The most definitive diagnostic tool is often a colonoscopy, where a flexible tube with a camera is inserted into the colon to examine the lining directly and take tissue biopsies. These biopsies are then analyzed under a microscope to confirm the type and extent of inflammation.
Treatment strategies for colitis are tailored to the specific type and severity of the condition. They can range from medications to surgical interventions:
| Treatment Category | Common Approaches | Purpose |
|---|---|---|
| Medications | Anti-inflammatory drugs (e.g., aminosalicylates), corticosteroids, immunosuppressants, biologics | Reduce inflammation, suppress immune response, promote healing |
| Antibiotics/Antivirals | Specific drugs for bacterial or viral infections | Eliminate infectious agents causing colitis |
| Surgery | Colectomy (removal of part or all of the colon) | For severe cases, complications, or when medical therapy fails |
| Nutritional Support | Dietary modifications, supplements, parenteral nutrition | Manage symptoms, prevent malnutrition, support healing |
The goal of treatment is to reduce inflammation, alleviate symptoms, prevent complications, and achieve long-term remission, particularly for chronic forms like ulcerative colitis or Crohn’s colitis.
Managing Colitis at Home
Learning how to manage colitis at home plays a significant role in improving quality of life and supporting medical treatments. While home management does not replace professional medical care, certain lifestyle adjustments can help alleviate symptoms and prevent flare-ups. Dietary modifications are often key; identifying and avoiding trigger foods can significantly reduce discomfort. Common triggers might include high-fiber foods, dairy, spicy foods, or caffeine, though individual responses vary.
Maintaining adequate hydration is crucial, especially for individuals experiencing diarrhea. Drinking plenty of water and electrolyte-rich fluids can help prevent dehydration. Stress management techniques, such as meditation, yoga, or deep breathing exercises, can also be beneficial, as stress is known to exacerbate symptoms in some people with inflammatory conditions.
Regular, moderate exercise, as advised by a healthcare provider, can contribute to overall well-being. It’s also vital to adhere strictly to prescribed medications and attend all follow-up appointments. Keeping a symptom diary can help track food triggers, stress levels, and medication effectiveness, providing valuable information for your healthcare team. Always consult with a doctor or registered dietitian before making significant changes to your diet or lifestyle to ensure they are appropriate for your specific condition.
