Cold Ischemia
Cold ischemia is a critical process in organ transplantation, involving the preservation of organs at low temperatures after their removal from a donor. This technique is fundamental to minimizing cellular damage and extending the viability of organs during transport and before implantation.
Key Takeaways
- Cold ischemia refers to the practice of cooling organs to reduce their metabolic rate post-excision.
- Its primary goal is to minimize cellular damage and extend the time organs can remain viable outside the body.
- While beneficial, prolonged cold ischemia can lead to various cellular injuries, impacting organ function after transplantation.
- Effective management of cold ischemia time is a crucial factor in the overall success of organ transplantation procedures.
What is Cold Ischemia?
Cold Ischemia refers to the period during which an organ is kept at hypothermic temperatures (typically between 0-8°C) after its blood supply has been interrupted and before its re-establishment in the recipient. This process is a cornerstone of modern organ transplantation, as it significantly slows down the metabolic processes within the cells, thereby reducing their demand for oxygen and nutrients. The primary aim of this technique is to preserve the structural integrity and functional capacity of the organ during the time it is transported from the donor to the recipient.
The concept of cold ischemia definition centers on leveraging reduced temperatures to mitigate the detrimental effects of oxygen deprivation. By lowering the temperature, cellular enzymatic reactions are decelerated, and the consumption of adenosine triphosphate (ATP), the cell’s primary energy currency, is dramatically decreased. This allows cells to survive for a longer duration without a continuous blood supply, providing a vital window for logistical coordination and surgical preparation in transplantation.
Effects of Cold Ischemia on Organ Viability
While essential for organ preservation, the duration and conditions of cold ischemia can have profound effects of cold ischemia on organs, influencing their viability and function post-transplantation. Despite the protective effects of hypothermia, cells still experience a degree of injury during this period. These injuries are often multifactorial, involving a complex interplay of biochemical and cellular changes that can compromise the organ’s ability to function optimally once reperfused.
Key cellular and molecular changes observed during cold ischemia include:
- ATP Depletion: Although slowed, ATP is still consumed, leading to eventual energy depletion, which impairs ion pump function and cellular homeostasis.
- Cell Swelling: Impaired ion pumps can lead to an influx of sodium and water into cells, causing cellular edema and potentially disrupting cell membranes.
- Oxidative Stress: Upon reperfusion (restoration of blood flow), the sudden reintroduction of oxygen can lead to the generation of reactive oxygen species, causing further cellular damage.
- Inflammation: Ischemic injury can trigger inflammatory responses, contributing to tissue damage and potentially leading to rejection or delayed graft function.
The extent of these effects varies significantly among different organs. For instance, kidneys generally tolerate longer cold ischemia times than hearts or lungs, which are more susceptible to ischemic injury. Understanding these organ-specific tolerances is crucial for optimizing preservation strategies and improving transplant outcomes.
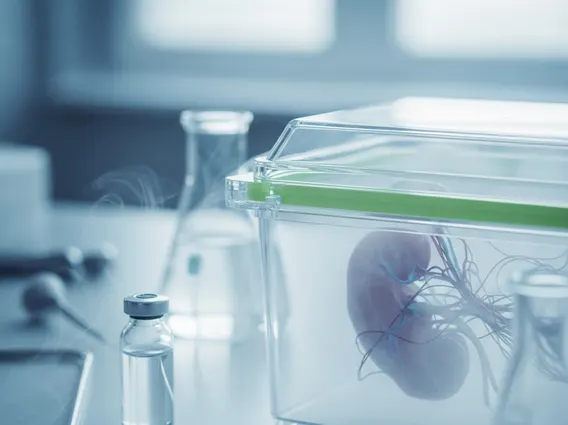
Cold Ischemia in Organ Transplantation
The management of cold ischemia in organ transplantation is a critical determinant of success, directly impacting graft survival and recipient outcomes. Following retrieval from the donor, organs are flushed with specialized preservation solutions and then stored in sterile containers on ice. These solutions, such as the University of Wisconsin (UW) solution, are designed to buffer pH, prevent cell swelling, and provide nutrients, further enhancing the protective effects of hypothermia.
The duration of cold ischemia, often referred to as ischemic time, is meticulously monitored. Shorter ischemic times are generally associated with better outcomes, as they minimize the cumulative cellular damage. For example, while kidney transplants can often tolerate cold ischemia times of 24 hours or more, heart and lung transplants typically aim for less than 4-6 hours due to the higher sensitivity of these organs to ischemic injury. According to data from the Organ Procurement and Transplantation Network (OPTN) and the United Network for Organ Sharing (UNOS), careful management of the entire transplant process, including cold ischemia, contributes to the generally high success rates observed in organ transplantation, with one-year graft survival rates for kidney transplants often exceeding 90% and liver transplants around 85% or higher, though these rates can vary by organ and recipient factors.
Ongoing research continues to explore novel preservation techniques, including machine perfusion, which circulates oxygenated preservation solutions through the organ at hypothermic or normothermic temperatures. These advancements aim to further extend preservation times, improve organ quality, and ultimately increase the availability of viable organs for transplantation, thereby enhancing patient lives.