Esophageal Cancer Treatment Options
Navigating a diagnosis of esophageal cancer can be overwhelming, but understanding the available esophageal cancer treatment options is a crucial first step. This article provides a comprehensive overview of the various therapeutic approaches, from traditional methods to the latest advancements, designed to help patients and their families make informed decisions.
Key Takeaways
- Esophageal cancer treatment is highly individualized, depending on the cancer’s stage, type, and the patient’s overall health.
- A multidisciplinary team approach, involving various specialists, is essential for developing the most effective treatment plan.
- Treatment modalities include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy, often used in combination.
- Early-stage cancers may be treated with less invasive methods, while advanced stages typically require more aggressive, multimodal approaches.
- Ongoing research continues to introduce latest esophageal cancer therapies, offering new hope and improved outcomes for patients.
Overview of Esophageal Cancer Treatment Options
The landscape of esophageal cancer treatment options overview is complex and highly personalized, reflecting the unique characteristics of each patient’s disease. Treatment decisions are made by a multidisciplinary team of specialists, including oncologists, surgeons, radiation oncologists, and gastroenterologists, who collaborate to devise the most effective strategy. This collaborative approach ensures that all aspects of the patient’s health and cancer specifics are considered.
Key factors influencing the choice of treatment include the stage of the cancer (how far it has spread), the type of esophageal cancer (adenocarcinoma or squamous cell carcinoma), the tumor’s location, and the patient’s overall health and preferences. The goal of treatment can range from curative intent, aiming to eliminate the cancer entirely, to palliative care, focused on managing symptoms and improving quality of life for advanced cases. The variety of available therapies means that patients have access to tailored plans that address their specific needs.
Understanding the types of esophageal cancer treatments available is fundamental. These can broadly be categorized into local treatments, which target the cancer directly in the esophagus, and systemic treatments, which affect cancer cells throughout the body. Often, a combination of these approaches is utilized to achieve the best possible outcomes.
| Treatment Modality | Primary Purpose | Description |
|---|---|---|
| Surgery (Esophagectomy) | Curative | Surgical removal of part or all of the esophagus, often with nearby lymph nodes. |
| Chemotherapy | Curative, Adjuvant, Palliative | Drugs that kill cancer cells, administered intravenously or orally. |
| Radiation Therapy | Curative, Palliative | High-energy rays to kill cancer cells or shrink tumors. |
| Targeted Therapy | Systemic | Drugs that specifically target cancer cells based on their genetic mutations. |
| Immunotherapy | Systemic | Boosts the body’s immune system to fight cancer cells. |
| Endoscopic Treatments | Curative (early-stage), Palliative | Minimally invasive procedures for very early cancers or symptom relief. |
Specific Treatment Modalities for Esophageal Cancer
A range of specific treatment modalities is employed in the fight against esophageal cancer, each with distinct mechanisms and applications. These treatments can be used individually or, more commonly, in combination to maximize their effectiveness and address different aspects of the disease. The choice of modality is carefully selected based on the cancer’s characteristics and the patient’s health profile.
Often, a multimodal approach is adopted, combining various therapies such as chemotherapy and radiation therapy (chemoradiation) before or after surgery. This strategy aims to shrink tumors, destroy microscopic cancer cells, and improve the chances of successful surgical removal, thereby enhancing long-term survival rates. The integration of different treatments underscores the aggressive nature of esophageal cancer and the need for comprehensive intervention.
Surgery for Esophageal Cancer
Surgery, primarily esophagectomy, is a cornerstone of curative esophageal cancer treatment for localized disease. This complex procedure involves removing the cancerous portion of the esophagus, along with surrounding lymph nodes, and then reconstructing the digestive tract, often using a section of the stomach or intestine. The extent of surgery depends on the tumor’s size and location, as well as the patient’s overall health and ability to tolerate a major operation.
While surgery offers the best chance for cure in eligible patients, it carries significant risks and potential complications. Advances in surgical techniques, including minimally invasive approaches, have aimed to reduce recovery times and improve patient outcomes. Post-operative care is critical and often involves a dedicated recovery period to manage pain, nutrition, and potential complications.
Systemic Therapies: Chemotherapy and Targeted Drugs
Chemotherapy for esophageal cancer information reveals its vital role in treating this disease, whether used alone or in combination with other therapies. Chemotherapy drugs work by killing rapidly dividing cells, including cancer cells, throughout the body. It can be administered before surgery (neoadjuvant) to shrink tumors, after surgery (adjuvant) to eliminate remaining cancer cells, or as a primary treatment for advanced or metastatic disease (palliative) to control growth and alleviate symptoms.
Beyond traditional chemotherapy, targeted therapy represents a more precise approach. These drugs specifically identify and attack cancer cells that have certain genetic mutations or protein overexpression, minimizing harm to healthy cells. Immunotherapy, another significant advancement, harnesses the body’s own immune system to recognize and destroy cancer cells. These innovative treatments are increasingly becoming part of the standard of care, particularly for patients with advanced disease or those who have not responded to conventional therapies.
Radiation therapy for esophageal cancer is another crucial component, often used in conjunction with chemotherapy (chemoradiation). This treatment uses high-energy rays to destroy cancer cells or shrink tumors. It can be delivered externally (external beam radiation therapy) or internally (brachytherapy). Radiation therapy can be curative for early-stage cancers, used before or after surgery, or employed palliatively to relieve symptoms such as difficulty swallowing or pain in advanced cases. Together, these systemic and localized treatments form the backbone of many esophageal cancer non-surgical treatments, offering diverse options for patients.
Tailoring Treatment by Esophageal Cancer Stage
The approach to esophageal cancer treatment is profoundly influenced by the stage of the disease, which describes how far the cancer has spread. Understanding the esophageal cancer treatment stages is critical for oncologists to develop an appropriate and effective treatment plan. Early detection often allows for less invasive and more curative options, while advanced stages typically require more aggressive and systemic interventions.
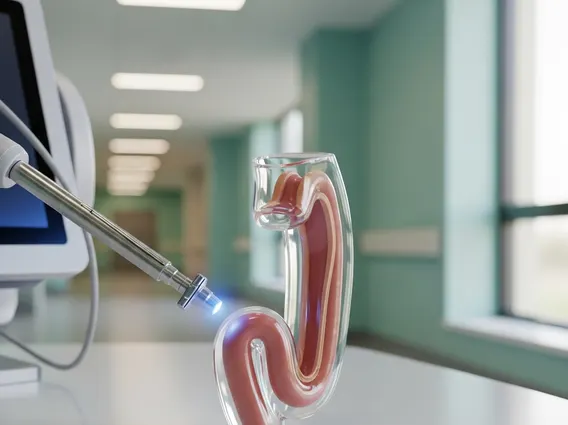
For very early-stage esophageal cancers, particularly those confined to the superficial layers of the esophagus, endoscopic treatments may be sufficient. Procedures like endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) can remove cancerous or pre-cancerous lesions without the need for major surgery. These minimally invasive techniques offer excellent outcomes for carefully selected patients, preserving the esophagus and reducing recovery time.
In cases of localized advanced disease, where the cancer has spread deeper into the esophageal wall or to nearby lymph nodes but not to distant organs, a multimodal approach is typically recommended. This often involves a combination of chemotherapy and radiation therapy (chemoradiation) followed by surgery (esophagectomy). The goal is to shrink the tumor, eliminate any microscopic spread, and then surgically remove the remaining cancer, aiming for a complete cure. This aggressive strategy has significantly improved survival rates for many patients.
For metastatic esophageal cancer, where the disease has spread to distant organs, the focus shifts towards systemic therapies and palliative care. Surgery is generally not curative in this setting. Instead, treatments like chemotherapy, targeted therapy, and immunotherapy are used to control cancer growth, manage symptoms, and improve the patient’s quality of life. Palliative radiation therapy may also be used to relieve symptoms such as pain or difficulty swallowing. Clinical trials often play a vital role for patients with advanced disease, offering access to cutting-edge treatments.
Latest Advances in Esophageal Cancer Therapy
The field of oncology is continuously evolving, and the latest esophageal cancer therapies offer renewed hope and improved outcomes for patients. These advancements are driven by a deeper understanding of the molecular biology of esophageal cancer, leading to more targeted and personalized treatment strategies. Research is focused on enhancing efficacy while minimizing side effects, ultimately improving both survival and quality of life.
One of the most significant breakthroughs has been the integration of immunotherapy into the treatment paradigm. Immunotherapy drugs, known as checkpoint inhibitors, work by unleashing the body’s own immune system to recognize and attack cancer cells. These therapies have shown promising results, particularly for patients with advanced esophageal cancer, offering durable responses in some individuals. Precision medicine, which involves tailoring treatment based on the specific genetic mutations or biomarkers found in a patient’s tumor, is also transforming care, allowing for the use of highly effective targeted therapies.
Furthermore, ongoing clinical trials are exploring novel drug combinations, advanced radiation techniques, and innovative surgical approaches. These studies are crucial for identifying new and more effective esophageal cancer treatment strategies. Patients are encouraged to discuss the possibility of participating in clinical trials with their healthcare team, as these can provide access to cutting-edge treatments that are not yet widely available. The continuous progress in research ensures that the future of esophageal cancer treatment is brighter than ever.
Frequently Asked Questions
What are the main factors influencing esophageal cancer treatment decisions?
Treatment decisions for esophageal cancer are highly individualized and depend on several key factors. These include the stage of the cancer (how far it has spread), the specific type of esophageal cancer (adenocarcinoma or squamous cell carcinoma), the tumor’s location, and the patient’s overall health status and preferences. A multidisciplinary team evaluates these elements to create a personalized treatment plan, aiming for the best possible outcome while considering the patient’s quality of life.
Can esophageal cancer be treated without surgery?
Yes, esophageal cancer non-surgical treatments are available and often effective, especially for early-stage disease or when surgery is not feasible. For very early cancers, endoscopic procedures can remove cancerous lesions. For more advanced but localized disease, a combination of chemotherapy and radiation therapy (chemoradiation) can be used with curative intent. For metastatic cancer, systemic therapies like chemotherapy, targeted therapy, and immunotherapy are primary treatments to control the disease and manage symptoms, without requiring surgery.
What is the role of immunotherapy in esophageal cancer?
Immunotherapy has emerged as a significant advancement in esophageal cancer treatment, particularly for advanced or metastatic cases. These treatments, often called checkpoint inhibitors, work by blocking proteins that prevent the immune system from attacking cancer cells. By removing these “brakes,” immunotherapy allows the body’s own immune cells to recognize and destroy the cancer. It offers a new avenue for treatment, sometimes providing durable responses and improved survival for patients who may not respond to traditional therapies.
