Living with Salivary Gland Cancer
A diagnosis of salivary gland cancer can be a life-altering event, bringing with it a unique set of challenges and questions. This article aims to provide a comprehensive guide for individuals navigating their journey, offering insights into understanding the diagnosis, managing daily life, building support, and embracing survivorship.
Key Takeaways
- Understanding your specific diagnosis and treatment plan is crucial for effective management and informed decision-making.
- Emotional support and practical coping strategies are vital from the moment of diagnosis through treatment and beyond.
- Adapting daily routines and proactively managing symptoms can significantly improve the quality of salivary gland cancer patient life.
- Building a strong network of peer and professional support is essential for navigating the complexities of the disease.
- Long-term follow-up and a focus on overall well-being are key to enhancing the quality of life for survivors.
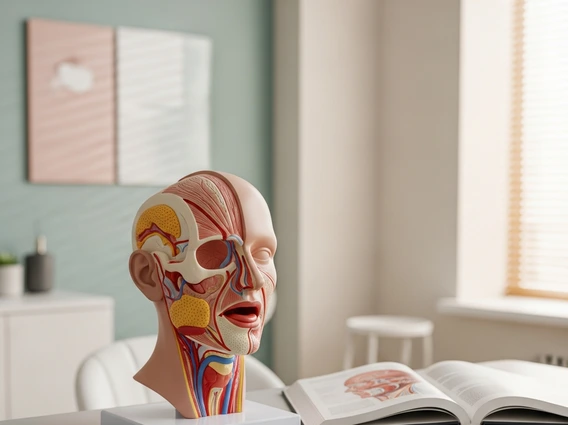
Understanding Your Diagnosis and Initial Steps
Receiving a cancer diagnosis, particularly for a less common type like salivary gland cancer, can be overwhelming. Salivary gland cancers are relatively rare, accounting for less than 1% of all cancers and approximately 6% of all head and neck cancers, according to the American Cancer Society. Understanding your specific type, stage, and prognosis is the first critical step in your journey toward living with salivary gland cancer.
Emotional Impact and Coping Strategies
The emotional impact of a cancer diagnosis can manifest in various ways, including shock, fear, anxiety, sadness, and even anger. It is entirely normal to experience a range of intense emotions. Effective coping with salivary gland cancer diagnosis involves acknowledging these feelings and seeking appropriate support. Many patients find solace in talking to trusted family members or friends, while others benefit from professional counseling or therapy. Mindfulness practices, meditation, and gentle exercise can also help manage stress and improve mental well-being during this challenging time.
Remember that your emotional health is as important as your physical health. Do not hesitate to reach out to mental health professionals who specialize in oncology support. They can provide strategies and resources tailored to your specific needs, helping you process the diagnosis and prepare for the journey ahead.
Initial Treatment Decisions and Planning
Once your diagnosis is confirmed, your medical team will discuss various treatment options. These often include surgery, radiation therapy, chemotherapy, or a combination of these, depending on the tumor’s characteristics and location. Actively participating in these discussions is vital. Ask questions, seek second opinions if desired, and ensure you understand the potential benefits and risks of each approach. This informed decision-making process empowers you and helps alleviate some of the uncertainty.
Developing a clear treatment plan with your oncology team is crucial. This plan will outline the sequence of treatments, expected timelines, and anticipated side effects. Early planning can also involve discussions about preserving quality of life, such as speech and swallowing function, which can be affected by treatments in the head and neck region.
Managing Daily Life with Salivary Gland Cancer
The journey through treatment and recovery often necessitates adjustments to your daily routine. Adapting to these changes is a significant part of living with salivary gland cancer and maintaining a sense of normalcy.
Practical Adjustments and Routine Changes
Cancer and its treatments can impact energy levels, appetite, and physical capabilities, requiring practical adjustments to your routine. For many, daily life with salivary gland cancer involves prioritizing rest, modifying work schedules, and delegating tasks. Nutritional changes may also be necessary, especially if treatments affect your ability to chew or swallow. Working with a dietitian can help ensure you maintain adequate nutrition and hydration. Simple changes, such as preparing meals in advance or accepting help from loved ones, can make a substantial difference in managing energy and maintaining independence.
It’s important to listen to your body and adjust your activities accordingly. Some days may be more challenging than others, and it’s okay to slow down. Establishing a new routine that accommodates your physical and emotional needs is key to navigating this period effectively.
Effective Symptom Management Strategies
Managing salivary gland cancer symptoms and treatment side effects is a continuous process that significantly impacts your well-being. Common symptoms and side effects can include dry mouth (xerostomia), pain, fatigue, changes in taste, and difficulty swallowing. Your medical team can offer various strategies to alleviate these issues.
- Dry Mouth: Use artificial saliva, sip water frequently, chew sugar-free gum, and avoid caffeine and alcohol.
- Pain: Work with your doctor to develop a pain management plan, which may include over-the-counter or prescription medications.
- Fatigue: Prioritize rest, engage in light exercise if approved by your doctor, and manage your schedule to conserve energy.
- Nausea: Anti-nausea medications, small frequent meals, and avoiding strong odors can help.
- Swallowing Difficulties: A speech therapist can provide exercises and strategies to improve swallowing function.
Open communication with your healthcare providers about any new or worsening symptoms is crucial. They can adjust your treatment plan or recommend additional interventions to enhance your comfort and quality of life.
Building a Robust Support System
No one should face cancer alone. Building a strong network of support is fundamental for individuals living with salivary gland cancer, providing emotional, practical, and informational assistance throughout their journey.
Connecting with Peer Support Groups
Connecting with others who have similar experiences can be incredibly empowering. Peer support groups offer a safe space to share feelings, exchange practical advice, and realize you are not alone. These groups, whether online forums or local in-person meetings, provide invaluable support for salivary gland cancer patients. Hearing from individuals who have navigated similar challenges can offer hope, perspective, and a sense of community. Many patients find that sharing their experiences and learning from others helps them cope with the emotional and practical aspects of their diagnosis and treatment.
Organizations dedicated to head and neck cancers often host such groups, providing a platform for patients and their families to connect. The shared understanding within these communities can be a powerful source of strength and resilience.
Professional and Community Resources
Beyond peer support, a wide array of professional and community resources can assist individuals and their families. Your oncology team, including nurses, social workers, and patient navigators, can guide you to relevant services. These may include:
- Financial Assistance Programs: Organizations that help with treatment costs, medication, or living expenses.
- Transportation Services: Programs that provide rides to and from appointments.
- Nutritional Counseling: Registered dietitians specializing in oncology can help manage dietary challenges.
- Psychological Support: Therapists and counselors who specialize in cancer care.
- Rehabilitation Services: Physical, occupational, and speech therapists to help regain function.
Exploring these resources for salivary gland cancer survivors and patients can significantly ease the burden of the disease, allowing you to focus on healing and recovery. Many hospitals and cancer centers have dedicated departments to help patients access these vital services.
Navigating Long-Term Effects and Survivorship
The journey doesn’t end with the completion of active treatment. Survivorship involves ongoing monitoring, managing potential long-term effects of salivary gland cancer, and focusing on overall well-being.
Post-Treatment Monitoring and Follow-Up
After treatment concludes, regular follow-up appointments are crucial. These typically involve physical examinations, imaging scans (such as MRI or CT), and blood tests to monitor for any signs of recurrence and to assess for late-onset side effects. The frequency of these appointments will gradually decrease over time, but consistent monitoring remains a cornerstone of survivorship care. Your oncology team will develop a personalized follow-up schedule based on your specific diagnosis and treatment.
It’s important to remain vigilant for any new symptoms or changes in your health and report them promptly to your healthcare provider. Early detection of any issues can lead to more effective management and better outcomes. Maintaining a healthy lifestyle, including a balanced diet and regular exercise, can also contribute to long-term health and reduce the risk of recurrence.
Enhancing Quality of Life Post-Treatment
Survivorship is about more than just being cancer-free; it’s about reclaiming and enhancing your quality of life. Many survivors experience lingering side effects such as fatigue, dry mouth, swallowing difficulties, or changes in taste, which can persist for months or even years. Proactive management of these issues is key. Rehabilitation services, including physical therapy, speech therapy, and occupational therapy, can help address functional impairments and improve daily living.
Psychological well-being is also paramount. Some survivors may experience anxiety, depression, or fear of recurrence. Continuing to engage with support groups or mental health professionals can provide valuable strategies for coping with these challenges. Focusing on hobbies, reconnecting with social activities, and setting new personal goals can help foster a sense of purpose and normalcy, allowing you to thrive as a survivor.
Frequently Asked Questions
What are common challenges in daily life for salivary gland cancer patients?
Patients often face challenges such as managing fatigue, coping with dry mouth (xerostomia) due to radiation, and adjusting to changes in taste or swallowing. Practical adjustments to diet, work schedules, and social activities become necessary. Maintaining energy levels and adapting routines to accommodate treatment side effects are central to navigating daily life with salivary gland cancer effectively. Open communication with healthcare providers helps address these issues.
How can I find effective support after a salivary gland cancer diagnosis?
Effective support for salivary gland cancer patients can be found through various channels. Connecting with peer support groups, either online or in person, offers a community of individuals with shared experiences. Additionally, your oncology team can direct you to professional resources such as social workers, patient navigators, and mental health specialists who provide tailored guidance and access to community services like financial aid or transportation assistance.
What are the key aspects of long-term follow-up for salivary gland cancer survivors?
Long-term follow-up for survivors involves regular medical check-ups, including physical exams and imaging, to monitor for recurrence and manage any persistent or late-onset side effects. Addressing long-term effects of salivary gland cancer, such as chronic dry mouth or swallowing issues, is crucial. Additionally, focusing on overall well-being, including psychological support and access to rehabilitation services, helps survivors enhance their quality of life and utilize available resources for salivary gland cancer survivors.