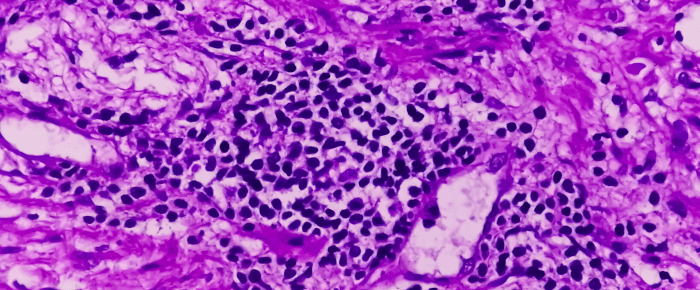
Multiple myeloma is the most common type of plasma cell cancer. Myeloma cells are abnormal plasms cells and are produced in the bones and bone marrow. These cells can eventually develop into tumors called plasmacytomas in many of the bones throughout the body.
Multiple myeloma is not considered a single disease, there are many subtypes that are either inactive or active. Active multiple myelomas are labeled as aggressive or non-aggressive based on the rate of growth and the spread of the cancer, as well as the symptoms and complications associated with the subtype. Myeloma subtypes are considered active if symptoms or organ damage from the disease have occurred.
Once the multiple myeloma diagnosis is confirmed, additional testing can determine the type of multiple myeloma present. These tests include:
- FISH analysis: Laboratory test to identify and count the genes or chromosomes in cancer cells. DNA containing fluorescent dyes are artificially made then added to the patient’s tumor samples. The DNA then binds to specific genes and chromosomes and light up when viewed under a microscope. This test helps doctors determine the appropriate treatment and confirm the subtype of multiple myeloma.
- Cytogenetics testing: The chromosomes in cancer cells are counted and checked for any alterations or damage. This test is used to diagnose cancer, determine the best treatment options, and monitor how well treatment is working.
- Gene expression profiling: This test is used as a tool for risk stratification for multiple myeloma by analyzing the genetic makeup of the myeloma cells present.
These tests identify the chromosomes and genes that are abnormal and helped grow the myeloma.
Once myeloma cells are abundant, it causes:
- Lower blood cell counts in the bone marrow
- Frequent infection
- Bone pain and discomfort
- Weakened bones that fracture easily
Osteoblasts and osteoclasts are 2 types of bone cells that are unable to function properly when the bones are weakened from the myeloma. Osteoblasts from bones and osteoclasts break down bone. Myeloma cells activate the osteoclasts and not the osteoblasts, causing the bone to break down at a faster rate. The myeloma cells are also divided into two main subtypes, hyperdiploid (HMM) and non-hyperdiploid. HMM myeloma cells have a higher number of chromosomes than normal and consists of nearly half of all myeloma cases. Non-hyperdiploid, also called hypodiploid, myeloma cells have less chromosomes than normal and are more aggressive than HMM cells, accounting for 40 percent of myeloma cases.
Light Chain Myeloma
About 15-20 percent of multiple myeloma cases are considered light chain myeloma, which describes patients who only form the light chain part of the immunoglobin and not the heavy chain.
Immunoglobins are antibodies made by myeloma cells. Light chains are smaller than M-proteins and can be detected more easily in urine than in blood, also known as Bence-Jones proteins. Once light chains reach the kidneys, they are filtered out of the blood. Without the heavy chain, the light chain can buildup in the kidneys leading to damage.
Non-Secretory Myeloma
Non-secretory myeloma is found in patients with myeloma cells that do not secrete enough M-proteins or light chains in the blood and urine to be detected by protein electrophoresis. X-rays in non-secretory myeloma patients will show osteolytic lesions in the bones. This subtype of multiple myeloma can be diagnosed with a bone marrow biopsy.
Solitary Plasmacytoma
Solitary plasmacytoma is an active type of myeloma that is a singular tumor from plasma cells located in the bone or nearby tissues. Having these tumors in multiple locations is multiple myeloma, one tumor is considered solitary plasmacytoma.
Treatment options for solitary plasmacytoma include radiation therapy, surgery, or in some cases both. Frequent checkups are necessary for patients due to the risk of solitary plasmacytoma developing into multiple myeloma.
The diagnostic tests for solitary plasmacytoma are the same as multiple myeloma, which require imaging of the bones are:
- PET scan
- CT scan
- MRI
Extramedullary Plasmacytoma
Extramedullary plasmacytoma consists of multiple tumors in the soft tissues outside the bone marrow, often in the nose, throat, sinus, or larynx. 30 percent of these cases develop into multiple myeloma. Treatment options for extramedullary plasmacytoma are like those of solitary plasmacytoma.
Monoclonal Gammopathy of Undetermined Significance (MGUS)
Monoclonal gammopathy of undetermined significance (MGUS) is an inactive myeloma that involves the abnormal antibodies and M-proteins, which can lead to active myeloma. However, the symptoms are not related to multiple myeloma. For those who have MGUS for 20 years, 20 percent of patients will develop active myeloma. Patients receive active monitoring from doctors with frequent checkups until symptoms worsen, such as pain, muscle weakness, bleeding, heart, kidney problems, or numbness in the feet, thighs, or hands. Doctors will also monitor the number of M-proteins and signs of organ damage.
Smoldering Multiple Myeloma (SMM)
Smoldering multiple myeloma (SMM) is an inactive precancerous form of myeloma that causes a higher-than-normal number of M-proteins in the blood or myeloma cells in the bone marrow. Half of all SMM patients develop multiple myeloma within 5 years Imaging tests can be used to diagnose and monitor the condition such as a skeletal survey, MRI, and a PET-CT scan.
Immunoglobulin D (IgD) Myeloma
Immunoglobulin D (IgD) myeloma is a rare active type of multiple myeloma that occurs in only 1 to 2 percent of all myeloma cases. Men under 60 are at the most risk of developing IgD myeloma.
Immunoglobulin E (IgE) Myeloma
Immunoglobulin E (IgE) myeloma is the rarest form of active myeloma but causes the same signs and symptoms as other subtypes of myeloma. IgE is more aggressive than other types, often spreading outside the bone marrow quickly and in some cases progresses to plasma cell leukemia.
Sources: