Total Body Irradiation
Total Body Irradiation (TBI) is a specialized form of radiation therapy used primarily as a conditioning regimen before a bone marrow or stem cell transplant. This intensive treatment aims to eliminate cancer cells and suppress the patient’s immune system, preparing the body for the new healthy cells.
Key Takeaways
- Total Body Irradiation (TBI) is a crucial pre-transplant treatment for certain cancers.
- It involves delivering radiation to the entire body to destroy cancer cells and suppress the immune system.
- The procedure is carefully planned and delivered in multiple fractions over several days.
- Patients may experience both acute (short-term) and chronic (long-term) side effects.
- TBI is a highly specialized therapy requiring a multidisciplinary medical team.
What is Total Body Irradiation (TBI)?
Total Body Irradiation (TBI) is a complex radiation therapy technique designed to treat certain types of cancer, particularly those requiring a stem cell or bone marrow transplant. Its primary purpose is twofold: to eradicate any remaining cancer cells throughout the body and to suppress the patient’s immune system. This immune suppression is vital to prevent the recipient’s body from rejecting the transplanted donor cells, a critical step in successful transplantation.
The application of total body irradiation for cancer is most commonly seen in patients with leukemias, lymphomas, multiple myeloma, and other hematologic malignancies. By targeting the entire body, TBI aims to reach cancer cells that may have spread beyond localized areas, which might not be accessible through conventional, localized radiation treatments. The specific dosage and fractionation (number of treatment sessions) are meticulously planned by a radiation oncologist, often in conjunction with a transplant team, to maximize therapeutic effect while minimizing damage to healthy tissues.
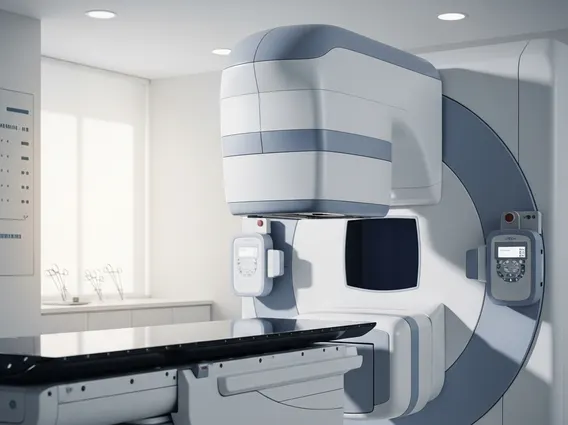
The Total Body Irradiation (TBI) Procedure
The total body irradiation procedure is a highly coordinated and precise process that typically spans several days. Before treatment begins, patients undergo extensive planning, including simulations and dosimetry, to determine the exact radiation fields, angles, and doses. This ensures that the radiation is delivered uniformly across the body while critical organs receive appropriate shielding or dose modulation. Patients are positioned carefully, often lying down or standing, at a specific distance from the radiation source to ensure even dose distribution.
TBI is usually delivered in multiple fractions, meaning the total radiation dose is divided into smaller, daily doses over several days. This fractionation allows healthy cells time to repair themselves between treatments, reducing the severity of side effects, while still being effective against cancer cells. Each treatment session can last from 20 minutes to over an hour, depending on the specific protocol. Throughout the procedure, the medical team closely monitors the patient, and adjustments are made as necessary to maintain accuracy and patient comfort. The entire process is a critical preparatory step before the infusion of new stem cells or bone marrow.
Potential Side Effects of Total Body Irradiation (TBI)
While Total Body Irradiation is a life-saving treatment for many, it is an intensive therapy that can lead to a range of side effects. These total body irradiation side effects can be broadly categorized into acute (short-term) and chronic (long-term) effects. Acute side effects typically manifest during or shortly after treatment and are often managed with supportive care. Chronic side effects can develop months or even years later and require ongoing monitoring.
Common acute side effects include:
- Nausea and vomiting
- Fatigue
- Hair loss
- Skin redness or irritation
- Mouth sores (mucositis)
- Diarrhea
- Temporary decrease in blood cell counts (myelosuppression)
Long-term side effects can be more severe and may include cataracts, lung damage (radiation pneumonitis), kidney damage, infertility, and an increased risk of developing secondary cancers. The medical team works diligently to mitigate these risks through careful planning, dose optimization, and supportive medications. Post-treatment, patients receive comprehensive follow-up care to monitor for and manage any emerging complications, ensuring the best possible long-term outcomes.
