Radical Cervicectomy
Radical Cervicectomy is a specialized surgical procedure primarily used to treat early-stage cervical cancer. It offers a unique approach by removing cancerous tissue while aiming to preserve a woman’s fertility.
Key Takeaways
- Radical Cervicectomy is a fertility-sparing surgical option for early-stage cervical cancer.
- The procedure involves removing the cervix, surrounding tissues, and often nearby lymph nodes.
- It can be performed via open, laparoscopic, or robot-assisted approaches.
- Recovery typically involves a hospital stay and several weeks of restricted activity.
- Potential side effects include infection, bleeding, and impacts on future pregnancies.
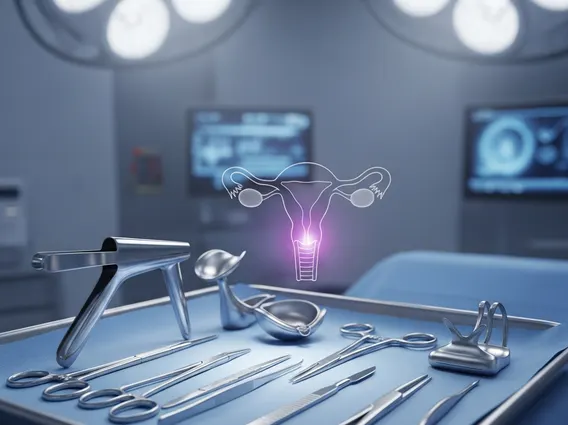
What is Radical Cervicectomy?
Radical Cervicectomy is a surgical procedure designed to treat specific types of early-stage cervical cancer. Unlike a hysterectomy, which removes the entire uterus, a radical cervicectomy focuses on excising the cervix, the upper part of the vagina, and the surrounding supportive tissues (parametria), while leaving the main body of the uterus intact. This approach is particularly significant for women who wish to preserve their ability to become pregnant in the future. The procedure also typically involves the removal of pelvic lymph nodes to check for cancer spread, which helps in determining further treatment needs.
Cervical cancer, the condition often necessitating this procedure, remains a global health concern. According to the World Health Organization (WHO), cervical cancer is the fourth most common cancer among women worldwide, with an estimated 604,000 new cases and 342,000 deaths in 2020. Identifying and treating the disease in its early stages is crucial for successful outcomes, and radical cervicectomy represents a vital option for eligible patients.
The Radical Cervicectomy Procedure
The **radical cervicectomy procedure explained** involves several key steps, performed under general anesthesia. The goal is to meticulously remove all cancerous tissue while minimizing impact on reproductive organs. There are different surgical approaches depending on the patient’s specific condition and the surgeon’s expertise:
- Abdominal (Open) Cervicectomy: This traditional method involves a larger incision in the abdomen, providing the surgeon with a direct view of the pelvic organs.
- Laparoscopic Cervicectomy: A minimally invasive approach where several small incisions are made, and a camera and specialized instruments are used to perform the surgery.
- Robotic-Assisted Laparoscopic Cervicectomy: Similar to laparoscopic surgery, but the instruments are controlled by a robotic system, offering enhanced precision and dexterity for the surgeon.
Regardless of the approach, the core steps include the removal of the cervix, the parametrial tissues, and a portion of the upper vagina. Pelvic lymph nodes are also often removed to check for microscopic cancer cells. After the cancerous tissue is removed, the remaining portion of the uterus is reconnected to the vagina, and a stitch (cerclage) may be placed to help support future pregnancies.
Radical Cervicectomy Recovery and Potential Side Effects
The **radical cervicectomy recovery time** varies significantly among individuals, but generally involves a hospital stay of a few days, followed by several weeks of recovery at home. During this period, patients are advised to limit physical activity, avoid heavy lifting, and refrain from sexual intercourse to allow the surgical sites to heal properly. Pain management is typically provided, and patients receive instructions on wound care and signs of complications to watch for.
While effective, the procedure can lead to various **radical cervicectomy side effects** and potential complications. These may include:
- Infection: At the surgical site or in the urinary tract.
- Bleeding: Both during and after the surgery.
- Damage to nearby organs: Such as the bladder or bowel, though rare.
- Lymphoedema: Swelling in the legs if a significant number of lymph nodes were removed.
- Changes in menstrual cycle: Though the uterus remains, some women may experience altered periods.
- Impact on fertility and pregnancy: While fertility is preserved, there is an increased risk of premature birth or miscarriage due to cervical incompetence in subsequent pregnancies.
Patients are closely monitored post-surgery, and follow-up appointments are crucial to assess healing, manage any side effects, and monitor for recurrence of cancer. Comprehensive discussions with the medical team before and after the procedure are essential for understanding the individual risks and benefits.
