Pseudomyxoma Peritonei
Pseudomyxoma Peritonei (PMP) is a rare clinical condition characterized by the accumulation of mucinous (jelly-like) material in the abdominal cavity. This condition typically originates from a ruptured appendix, though other primary sites are possible.
Key Takeaways
- Pseudomyxoma Peritonei (PMP) is a rare, slow-growing cancer-like condition involving mucus accumulation in the abdomen.
- It most commonly originates from a ruptured appendix, spreading mucinous cells throughout the peritoneal cavity.
- Symptoms often develop subtly and include abdominal distension, pain, and changes in bowel habits.
- Diagnosis involves imaging scans, biopsies, and sometimes exploratory surgery.
- Treatment primarily focuses on cytoreductive surgery (CRS) combined with hyperthermic intraperitoneal chemotherapy (HIPEC).
What is Pseudomyxoma Peritonei (PMP)?
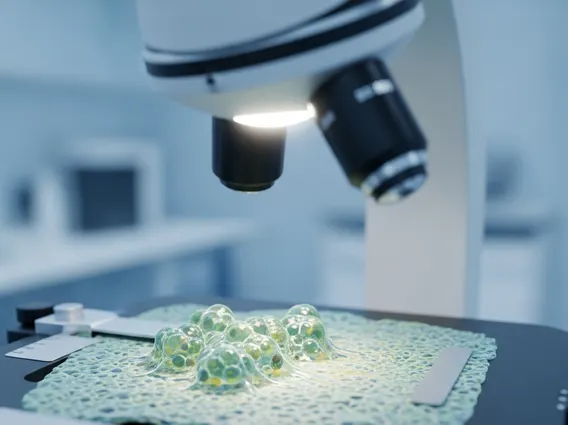
Pseudomyxoma Peritonei (PMP) is a rare, chronic condition characterized by the progressive accumulation of mucinous material within the peritoneal cavity, which is the space between the abdominal organs. Often described as “jelly belly,” this condition is typically caused by a ruptured mucinous tumor, most commonly originating from the appendix. The cells from this tumor spread throughout the abdomen, producing mucus that can encapsulate organs, leading to their compression and impaired function. PMP is considered a low-grade malignancy, meaning it grows slowly and rarely metastasizes to distant organs, but its local spread can be extensive and debilitating.
The exact prevalence of PMP is challenging to determine due to its rarity, but it is considered an extremely rare condition, affecting a very small percentage of the population annually. This condition primarily affects adults, with a slight predominance in women. Understanding PMP is crucial for early detection and management, as its insidious onset often leads to delayed diagnosis.
Pseudomyxoma Peritonei Symptoms, Signs, and Causes
The development of pseudomyxoma peritonei symptoms and signs is often gradual and non-specific, making early diagnosis challenging. As the mucinous material accumulates, it can lead to a range of discomforts. Common symptoms include increasing abdominal girth or distension, vague abdominal pain or discomfort, and changes in bowel habits such as constipation or diarrhea. Patients may also experience nausea, vomiting, loss of appetite, and unintended weight loss. In some cases, a palpable abdominal mass might be present. Women may experience new-onset hernias or ovarian masses, which can sometimes be mistaken for other conditions.
The primary pseudomyxoma peritonei causes and risk factors involve the rupture of a mucinous tumor, most frequently from the appendix. This rupture allows mucin-producing epithelial cells to disseminate into the peritoneal cavity. While appendiceal mucinous neoplasms are the most common origin, PMP can also arise, albeit rarely, from other sites such as the colon, stomach, pancreas, gallbladder, or ovaries. The exact mechanisms that trigger the initial mucinous tumor formation are not fully understood, but genetic factors and certain inflammatory conditions are being investigated. There are no known modifiable risk factors for PMP, emphasizing the importance of recognizing its subtle symptoms for timely medical evaluation.
Pseudomyxoma Peritonei Treatment Options
Effective pseudomyxoma peritonei treatment options are complex and typically involve a multidisciplinary approach due to the condition’s unique characteristics. The cornerstone of treatment is a specialized surgical procedure known as cytoreductive surgery (CRS), often combined with hyperthermic intraperitoneal chemotherapy (HIPEC).
- Cytoreductive Surgery (CRS): This extensive surgical procedure aims to remove as much of the visible mucinous tumor and affected tissue as possible from the abdominal cavity. This can involve removing parts of affected organs, such as the omentum, spleen, gallbladder, and sections of the bowel. The goal is to leave no macroscopic disease behind.
- Hyperthermic Intraperitoneal Chemotherapy (HIPEC): Immediately following CRS, a heated chemotherapy solution is circulated throughout the abdominal cavity for a short period. The heat enhances the penetration and efficacy of the chemotherapy drugs, targeting any remaining microscopic cancer cells while minimizing systemic side effects.
Other potential treatments, depending on the extent of the disease and patient health, may include systemic chemotherapy, though it is generally less effective for PMP due to the localized nature of the disease and the protective barrier of the mucus. In some cases, palliative care may be considered to manage symptoms and improve quality of life, especially for advanced or recurrent disease that is not amenable to further surgical intervention. Regular follow-up with imaging and tumor markers is essential after treatment to monitor for recurrence.
