Precursor T Lymphoblastic Leukemia
Precursor T Lymphoblastic Leukemia is an aggressive form of blood cancer that originates in the bone marrow, affecting the development of T-lymphocytes. This condition requires prompt and specialized medical attention due to its rapid progression.
Key Takeaways
- Precursor T Lymphoblastic Leukemia (PT-ALL) is a fast-growing cancer of immature T-cells in the bone marrow and blood.
- Symptoms often include fatigue, fever, bruising, and enlarged lymph nodes or a mediastinal mass.
- Diagnosis involves bone marrow biopsy, blood tests, and advanced cellular and genetic analyses.
- Treatment typically includes intensive chemotherapy, and sometimes stem cell transplantation or targeted therapies.
- Early diagnosis and a comprehensive treatment plan are crucial for managing PT-ALL.
What is Precursor T Lymphoblastic Leukemia?
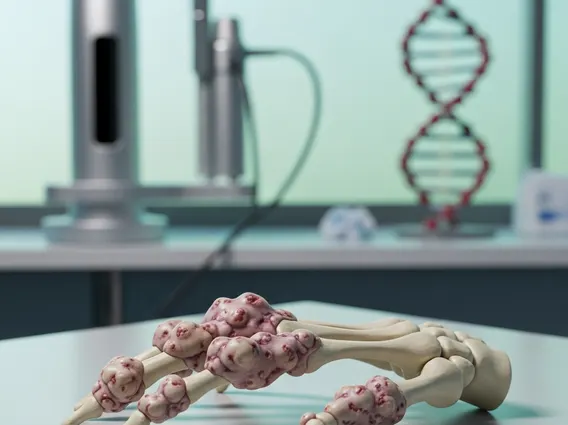
Precursor T Lymphoblastic Leukemia (PT-ALL) is a rare and aggressive type of acute lymphoblastic leukemia (ALL) that specifically affects the T-lymphocyte lineage. It originates when immature white blood cells, called lymphoblasts, become cancerous and multiply uncontrollably in the bone marrow. These abnormal cells, known as T-lymphoblasts, fail to mature properly and accumulate, crowding out healthy blood cells. This impairs the bone marrow’s ability to produce normal red blood cells, white blood cells, and platelets, leading to various health complications.
PT-ALL accounts for approximately 15% of all ALL cases in children and 25% in adults, making it a significant subtype within the broader ALL spectrum. Its aggressive nature necessitates intensive treatment strategies. The disease can spread rapidly from the bone marrow to other parts of the body, including the lymph nodes, spleen, liver, central nervous system, and thymus, which is often involved due to its role in T-cell development. (Source: American Cancer Society, general statistics on ALL subtypes).
Symptoms and Diagnosis of Precursor T Lymphoblastic Leukemia
The precursor t-all symptoms are often non-specific and can mimic those of other common illnesses, making early detection challenging. These symptoms typically arise from the bone marrow’s inability to produce sufficient healthy blood cells. Patients may experience persistent fatigue and weakness due to anemia (low red blood cells), frequent infections and fevers caused by a compromised immune system (low healthy white blood cells), and easy bruising or bleeding due to thrombocytopenia (low platelets). Additionally, the accumulation of leukemic cells can lead to swollen lymph nodes, an enlarged liver or spleen, and bone or joint pain. A distinctive feature in many PT-ALL cases is the presence of a mediastinal mass, a tumor in the chest that can cause breathing difficulties, coughing, or swelling in the face and neck.
Diagnosing precursor t lymphoblastic leukemia involves a series of comprehensive tests to confirm the presence of leukemic cells and determine their specific type. The diagnostic process typically includes:
- Complete Blood Count (CBC): Reveals abnormalities in blood cell counts, such as very high or very low white blood cell counts, anemia, and thrombocytopenia.
- Bone Marrow Aspiration and Biopsy: This is the definitive diagnostic procedure, where samples of bone marrow are taken from the hip bone to examine for the presence and percentage of lymphoblasts.
- Immunophenotyping: This technique uses flow cytometry to identify specific markers on the surface of the leukemic cells, confirming their T-cell lineage and immaturity.
- Cytogenetic and Molecular Genetic Testing: These tests analyze the chromosomes and genes within the leukemic cells for specific abnormalities, which are crucial for prognosis and guiding treatment decisions.
- Lumbar Puncture (Spinal Tap): Performed to check if leukemia cells have spread to the central nervous system.
Treatment Options for Precursor T Lymphoblastic Leukemia
Effective management of precursor t-all treatment options requires an aggressive and multi-phase approach, often involving a combination of therapies. The primary goal is to eradicate the leukemic cells and prevent relapse. Treatment protocols are highly individualized, based on factors such as the patient’s age, overall health, specific genetic abnormalities found in the leukemia cells, and whether the disease has spread to the central nervous system.
The mainstays of treatment include:
- Intensive Chemotherapy: This is the cornerstone of PT-ALL treatment, typically administered in several phases (induction, consolidation, interim maintenance, and maintenance) over a period of two to three years. It involves powerful drugs designed to kill rapidly dividing cancer cells throughout the body.
- Stem Cell Transplantation (SCT): For patients with high-risk features or those who relapse, an allogeneic (donor) stem cell transplant may be considered. This procedure replaces the patient’s diseased bone marrow with healthy stem cells from a donor.
- Targeted Therapies: These newer drugs specifically target molecular pathways or proteins involved in cancer growth, often used in conjunction with chemotherapy or for relapsed/refractory cases.
- Immunotherapy: Approaches like CAR T-cell therapy, which genetically engineers a patient’s own T-cells to recognize and attack cancer cells, are emerging as promising options for certain types of ALL, including PT-ALL, especially in relapsed settings.
- Central Nervous System (CNS) Prophylaxis: Because PT-ALL can spread to the brain and spinal cord, treatment often includes intrathecal chemotherapy (chemotherapy injected directly into the spinal fluid) or radiation therapy to the brain to prevent or treat CNS involvement.
The treatment journey for Precursor T Lymphoblastic Leukemia is complex and requires close monitoring by a team of oncology specialists to manage side effects and optimize outcomes.