Pomalidomide
Pomalidomide is a medication primarily used in the field of oncology, specifically for the treatment of certain blood cancers. It belongs to a class of drugs known as immunomodulatory drugs, which exert their therapeutic effects through complex interactions with both cancer cells and the immune system.

Key Takeaways
- Pomalidomide is an immunomodulatory drug (IMiD) used in oncology.
- It is primarily indicated for treating relapsed and refractory multiple myeloma.
- Its mechanism involves degrading specific cancer-promoting proteins and modulating immune responses.
- Benefits include improved survival rates for patients with advanced disease.
- Common side effects include fatigue, low blood counts, and an increased risk of blood clots.
What is Pomalidomide?
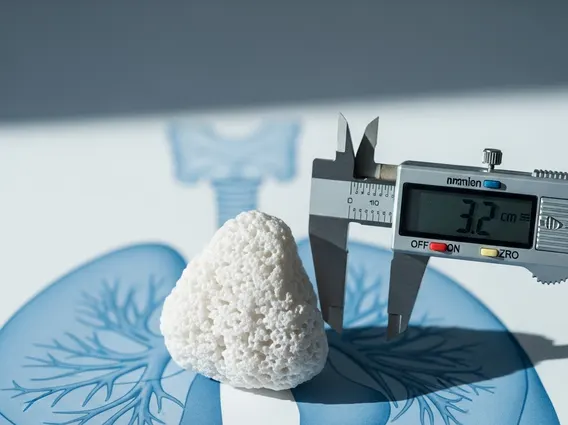
Pomalidomide is an immunomodulatory agent (IMiD) specifically designed for the treatment of certain hematologic malignancies. As a derivative of thalidomide, it has been developed to offer enhanced anti-cancer activity and a distinct safety profile. This medication is administered orally, making it a convenient option for patients. Comprehensive pomalidomide drug information highlights its classification as an IMiD, its oral route of administration, and its critical role in advanced oncology settings, particularly for conditions that have become resistant to other treatments. It represents a significant therapeutic advancement for patients with limited options.
How Pomalidomide Works: Mechanism of Action
The mechanism by which Pomalidomide works is multifaceted, targeting both cancer cells directly and modulating the immune system. Pomalidomide primarily functions by binding to the cereblon (CRBN) protein, which is a key component of an E3 ubiquitin ligase complex. This binding event is crucial as it leads to the targeted degradation of specific proteins that are essential for the survival and proliferation of cancer cells.
Specifically, Pomalidomide promotes the degradation of the transcription factors Ikaros (IKZF1) and Aiolos (IKZF3). These proteins are vital for the growth and survival of multiple myeloma cells. By eliminating these factors, Pomalidomide effectively disrupts the cancer cell cycle and induces apoptosis (programmed cell death).
Furthermore, Pomalidomide modulates the immune system by enhancing the activity of T-cells and natural killer (NK) cells, which are critical components of the body’s anti-cancer defense. Concurrently, it suppresses the production of pro-inflammatory cytokines, creating a less hospitable environment for tumor growth. This dual action of direct cytotoxicity and immune system modulation underscores how Pomalidomide works to combat the disease.
Pomalidomide: Uses, Benefits, and Side Effects
Pomalidomide is primarily indicated for the treatment of adult patients with relapsed and refractory multiple myeloma. This means it is typically used after patients have received at least two prior therapies, including lenalidomide and a proteasome inhibitor, and have demonstrated disease progression on or within 60 days of completion of the last therapy. It is often prescribed in combination with dexamethasone to enhance its therapeutic effect.
The benefits of Pomalidomide are significant for patients facing advanced multiple myeloma, a challenging blood cancer. Clinical trials have consistently shown that Pomalidomide can improve progression-free survival and overall survival in these patients, offering a crucial treatment avenue when other options have been exhausted. For instance, studies have reported objective response rates ranging from 20-30% in highly pre-treated patient populations, providing a meaningful extension of life and improvement in quality of life for many. (Source: Based on data from pivotal clinical trials supporting FDA and EMA approvals, e.g., MM-003 trial).
Like all potent medications, Pomalidomide is associated with potential side effects. Patients receiving this medication require regular monitoring of blood counts and close observation for adverse reactions. Common side effects include:
- Fatigue and generalized weakness
- Myelosuppression, leading to low blood cell counts such as neutropenia (low white blood cells) and thrombocytopenia (low platelets), increasing infection and bleeding risks.
- Constipation and other gastrointestinal disturbances
- Peripheral neuropathy, characterized by numbness, tingling, or pain in the hands and feet
- Increased risk of venous thromboembolism (blood clots), which often necessitates concomitant anticoagulant therapy to mitigate this risk.