Polysomnogram
A Polysomnogram is a comprehensive diagnostic tool used to record various physiological parameters during sleep. This overnight study helps healthcare professionals identify and understand underlying sleep disorders that can significantly impact an individual’s health and quality of life.

Key Takeaways
- A Polysomnogram (PSG) is an overnight sleep study that monitors brain waves, breathing, heart rate, and other bodily functions.
- Its primary purpose is to diagnose a wide range of sleep disorders, including sleep apnea, narcolepsy, and restless legs syndrome.
- The procedure involves attaching sensors to the body in a specialized sleep lab to collect detailed data throughout the night.
- The information gathered from a PSG is crucial for developing effective treatment plans for sleep-related conditions.
What is a Polysomnogram (PSG)?
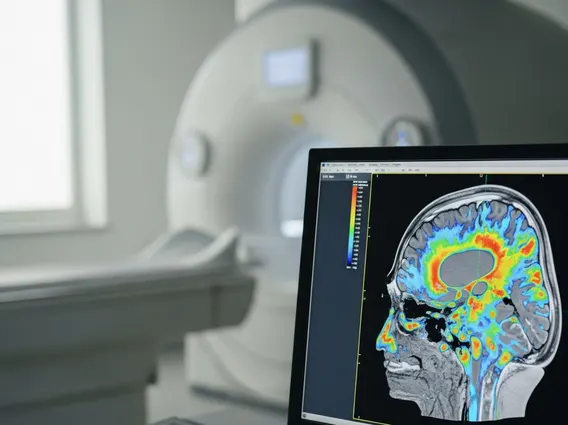
A Polysomnogram (PSG) is a non-invasive, overnight test that comprehensively records physiological data while a person sleeps. Often referred to simply as a sleep study, it is considered the gold standard for diagnosing many sleep-related conditions. During a PSG, specialized sensors are used to monitor several bodily functions, providing a detailed picture of an individual’s sleep architecture and any abnormalities that may occur.
The key parameters measured during a PSG include brain wave activity (electroencephalogram or EEG), eye movements (electrooculogram or EOG), muscle activity (electromyogram or EMG), heart rate (electrocardiogram or ECG), breathing patterns, oxygen saturation levels in the blood, and limb movements. By analyzing these synchronized recordings, sleep specialists can identify specific events and patterns indicative of various sleep disorders, which are often not apparent during wakefulness.
Purpose of Polysomnography and Conditions Diagnosed
The primary purpose of polysomnography is to accurately diagnose and characterize sleep disorders that can disrupt restorative sleep and lead to significant health issues. These disorders often manifest with symptoms like excessive daytime sleepiness, loud snoring, pauses in breathing, or difficulty falling or staying asleep. A PSG provides objective data that cannot be obtained through a simple physical examination or patient history alone.
Polysomnography is instrumental in diagnosing a variety of conditions, including:
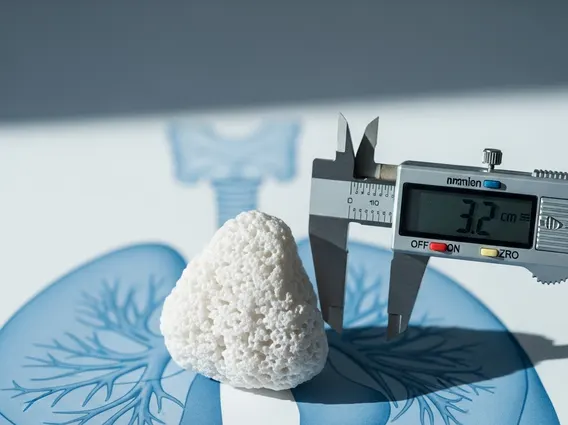
- Sleep Apnea: Both obstructive sleep apnea (OSA), characterized by repeated pauses in breathing due to airway collapse, and central sleep apnea (CSA), where the brain fails to send proper signals to breathing muscles. According to the American Academy of Sleep Medicine, approximately 30 million adults in the U.S. have sleep apnea, with many remaining undiagnosed.
- Narcolepsy: A chronic neurological condition causing overwhelming daytime sleepiness and sudden attacks of sleep.
- Restless Legs Syndrome (RLS): A neurological disorder characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations.
- Insomnia: Persistent difficulty with sleep initiation, duration, consolidation, or quality.
- Parasomnias: Disruptive sleep-related events such as sleepwalking, night terrors, or REM sleep behavior disorder.
The detailed insights gained from a PSG allow clinicians to differentiate between various sleep problems and tailor appropriate treatment strategies, significantly improving patient outcomes and overall well-being.
How a Polysomnogram Procedure Works
The polysomnogram procedure explained typically begins with preparation at home, where patients are usually advised to avoid caffeine and alcohol on the day of the study, as these substances can interfere with sleep patterns. Upon arrival at a sleep center or lab in the evening, a trained technologist will guide the patient through the process.
Sensors are carefully attached to specific areas of the body using adhesive or paste. These include electrodes on the scalp to measure brain waves, near the eyes for eye movements, on the chin for muscle activity, and on the chest for heart rate. Belts are placed around the chest and abdomen to monitor breathing effort, while a small device is clipped to a finger to measure blood oxygen levels. Airflow sensors are also placed near the nose and mouth. This comprehensive setup is essentially how a sleep study works, ensuring that a wide array of physiological data is captured.
Once the sensors are in place, the patient is encouraged to sleep as naturally as possible in a private room. Throughout the night, the technologist monitors the data from an adjacent control room. The collected information is then analyzed by a sleep specialist, who interprets the findings to provide a diagnosis and recommend a suitable treatment plan.