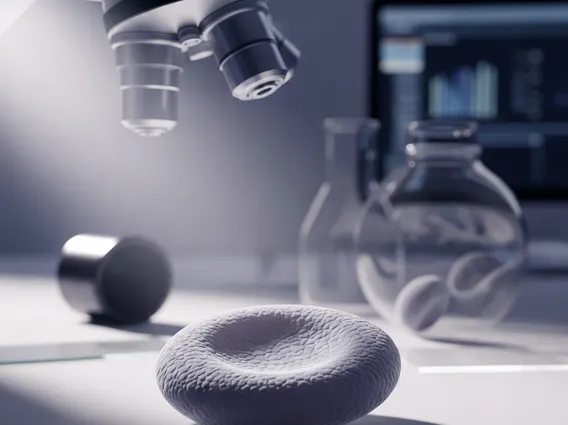
Platelet
Platelets are tiny, colorless cell fragments found in the blood that play a crucial role in the body’s natural healing process, particularly in stopping bleeding. They are essential for maintaining vascular integrity and preventing excessive blood loss.
Key Takeaways
- Platelets are small blood cell fragments vital for blood clotting and wound healing.
- They respond to blood vessel injuries by forming a plug, initiating the complex process of hemostasis.
- Platelet function in blood clotting involves adhesion, activation, and aggregation at the site of injury.
- Low platelet count causes (thrombocytopenia) can range from decreased production in the bone marrow to increased destruction in the bloodstream.
- Maintaining a healthy platelet count is critical for preventing both excessive bleeding and inappropriate clotting.
What is a Platelet?
A Platelet, also known as a thrombocyte, is a small, anucleated (lacking a nucleus) cell fragment that circulates in the blood. These fragments are produced in the bone marrow from large cells called megakaryocytes. Their primary function is to help stop bleeding by forming a plug at the site of an injured blood vessel. While often referred to as blood cells, platelets are technically cell fragments, measuring only about 2-3 micrometers in diameter. They have a lifespan of approximately 8 to 10 days before being removed by the spleen and liver. The normal range for platelet count in healthy individuals typically falls between 150,000 and 450,000 platelets per microliter of blood.
Platelet Function and Blood Clotting
The intricate process of hemostasis, or the cessation of bleeding, relies heavily on platelet function in blood clotting. When a blood vessel is damaged, platelets are rapidly activated and respond to the injury site. This response involves several key steps:
- Adhesion: Platelets first adhere to the exposed collagen in the damaged vessel wall, a process mediated by von Willebrand factor.
- Activation: Upon adhesion, platelets become activated, changing shape and releasing signaling molecules such as ADP and thromboxane A2. These molecules recruit more platelets to the site and promote further activation.
- Aggregation: Activated platelets then aggregate, or clump together, forming a primary platelet plug that physically seals the breach in the blood vessel. This plug provides a temporary barrier against blood loss.
- Coagulation Cascade: Simultaneously, platelets provide a surface for the activation of clotting factors, which leads to the formation of fibrin strands. These fibrin strands create a stable meshwork that reinforces the platelet plug, forming a robust blood clot. This entire coordinated effort ensures effective wound healing and prevents excessive bleeding.
This complex interplay demonstrates precisely how platelets work in the body to maintain circulatory integrity.
Causes of Low Platelet Count
A condition known as thrombocytopenia occurs when an individual has a low platelet count causes, meaning fewer than 150,000 platelets per microliter of blood. This can lead to an increased risk of bleeding and bruising. The causes of low platelet count are diverse and can generally be categorized into two main groups: decreased production of platelets in the bone marrow or increased destruction or sequestration of platelets in the bloodstream.
Common causes of decreased platelet production include:
- Bone Marrow Disorders: Conditions like leukemia, aplastic anemia, or myelodysplastic syndromes can impair the bone marrow’s ability to produce megakaryocytes, and thus platelets.
- Chemotherapy and Radiation: Cancer treatments often suppress bone marrow activity, leading to a temporary reduction in platelet production.
- Viral Infections: Certain viral infections, such as dengue fever, hepatitis C, HIV, and measles, can temporarily suppress platelet production or increase their destruction.
- Nutritional Deficiencies: Severe deficiencies in vitamin B12 or folate can also impact platelet production.
Causes related to increased platelet destruction or sequestration include:
- Immune Thrombocytopenia (ITP): An autoimmune disorder where the body’s immune system mistakenly attacks and destroys its own platelets. According to various health organizations, ITP affects approximately 1 in 10,000 to 1 in 20,000 adults annually.
- Medications: Certain drugs, including some antibiotics, anticoagulants, and diuretics, can trigger an immune response that destroys platelets.
- Enlarged Spleen (Splenomegaly): An enlarged spleen can trap and destroy an excessive number of platelets, leading to a lower count in circulation.
- Severe Infections (Sepsis): Widespread infection can lead to increased platelet consumption and destruction.
- Disseminated Intravascular Coagulation (DIC): A severe condition where blood clots form throughout the body, consuming platelets and clotting factors rapidly.
Identifying the specific cause of a low platelet count is essential for effective treatment and management.
