Peripheral Venous Catheter
A peripheral venous catheter is a common medical device used for various therapeutic and diagnostic purposes. Understanding its function, proper insertion, and potential complications is crucial for patient safety and effective healthcare delivery.
Key Takeaways
- A Peripheral Venous Catheter (PVC) is a small, flexible tube inserted into a peripheral vein, primarily for short-term access.
- PVCs are widely used for administering fluids, medications, and drawing blood samples.
- Proper insertion technique is vital to minimize pain and reduce the risk of complications.
- Common risks include infection, phlebitis, infiltration, and occlusion, requiring careful monitoring.
- Effective management of PVCs involves aseptic technique, regular assessment, and timely removal.
What is a Peripheral Venous Catheter (PVC)?
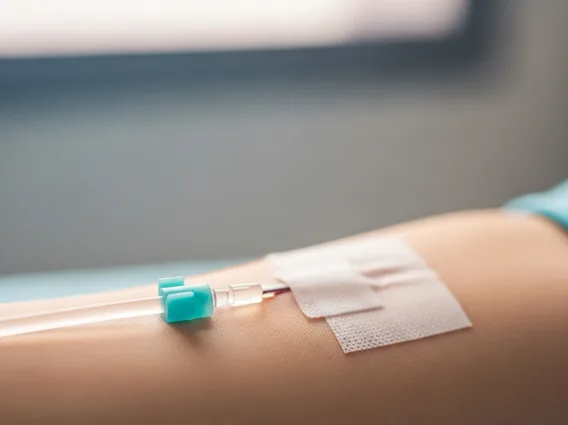
A Peripheral Venous Catheter (PVC) is a short, flexible tube inserted into a peripheral vein, typically in the arm or hand, to provide direct access to the bloodstream. This device is one of the most frequently used invasive medical tools in healthcare settings worldwide, with an estimated 300 million sold annually in the United States alone, according to the CDC. PVCs are designed for temporary use, usually for a few days, to facilitate the delivery of fluids, medications, and blood products, or to collect blood samples for diagnostic testing. They are distinct from central venous catheters, which are longer and inserted into larger veins closer to the heart for longer-term or more intensive treatments.
The primary purpose of a peripheral venous catheter is to establish a reliable and safe conduit for intravenous (IV) therapy. Its design allows for relatively straightforward insertion and removal, making it a cornerstone of modern medical practice. The choice of catheter size depends on the patient’s age, vein size, and the intended use, with larger gauges typically used for rapid fluid administration or blood transfusions, and smaller gauges for routine medication delivery.
Insertion, Uses, and Potential Risks of PVCs
How to Insert a Peripheral Venous Catheter
Inserting a peripheral venous catheter is a common procedure performed by trained healthcare professionals. The process begins with selecting an appropriate vein, usually in the non-dominant arm, considering factors like vein size, patient comfort, and the duration of therapy. After thoroughly cleaning the insertion site with an antiseptic solution, a tourniquet is applied to distend the vein. The catheter, which consists of a needle surrounded by a plastic cannula, is then carefully advanced into the vein. Once blood return is observed, indicating successful venipuncture, the needle is withdrawn, leaving the flexible cannula in place. The catheter is then secured with a dressing, and the site is labeled with the date and time of insertion. Adherence to strict aseptic technique throughout the procedure is paramount to prevent infection.
The peripheral venous catheter uses and risks are extensive. PVCs are indispensable for a wide range of medical applications, including:
- Administering intravenous fluids for hydration or electrolyte replacement.
- Delivering medications, such as antibiotics, analgesics, and chemotherapy agents.
- Infusing blood products, including packed red blood cells, platelets, and plasma.
- Obtaining venous blood samples for diagnostic laboratory tests.
- Providing nutritional support through parenteral nutrition in certain cases.
Despite their widespread utility, PVCs carry inherent risks. The most common immediate risks include pain, bruising, and hematoma formation at the insertion site. More serious potential risks involve accidental arterial puncture, nerve damage, or allergic reactions to materials or antiseptics. Proper training and careful technique significantly mitigate these risks.
Managing Peripheral Venous Catheter Complications
Effective management of PVCs involves continuous monitoring to prevent and address potential issues. Peripheral venous catheter complications can range from mild to severe and require prompt recognition and intervention. One of the most common complications is phlebitis, which is inflammation of the vein, often presenting as redness, warmth, pain, and a palpable cord along the vein. Infiltration occurs when the catheter dislodges from the vein, and fluids or medications leak into the surrounding tissue, causing swelling and discomfort. Extravasation is a more severe form of infiltration involving vesicant (blister-causing) drugs, which can lead to tissue damage.
Infection is another significant concern, ranging from local site infection to more serious bloodstream infections. The risk of infection is estimated to be low for peripheral catheters, with rates typically less than 0.1% per catheter-day, but it increases with prolonged dwell time and poor aseptic technique. Occlusion, or blockage of the catheter, can occur due to blood clots or precipitation of incompatible medications. Regular flushing of the catheter helps maintain patency. To minimize complications, healthcare providers adhere to best practices such as:
- Using aseptic technique during insertion and dressing changes.
- Regularly assessing the insertion site for signs of inflammation, infection, or infiltration.
- Removing the catheter promptly when no longer needed or at the first sign of complications.
- Educating patients on signs and symptoms to report.
By following these guidelines, the safety and efficacy of peripheral venous catheters can be maximized, ensuring optimal patient care.
