Pericardial Tamponade
Pericardial tamponade is a life-threatening medical emergency where fluid accumulates in the pericardial sac, compressing the heart and impairing its ability to pump blood. Understanding this critical condition is crucial for timely diagnosis and intervention.
Key Takeaways
- Pericardial tamponade is a critical condition caused by rapid fluid buildup around the heart.
- It severely restricts the heart’s pumping action, leading to reduced blood flow to the body.
- Symptoms often include shortness of breath, chest pain, and signs of shock.
- Diagnosis relies heavily on imaging like echocardiography and clinical assessment.
- Emergency treatment typically involves pericardiocentesis to drain the accumulated fluid.
What is Pericardial Tamponade?
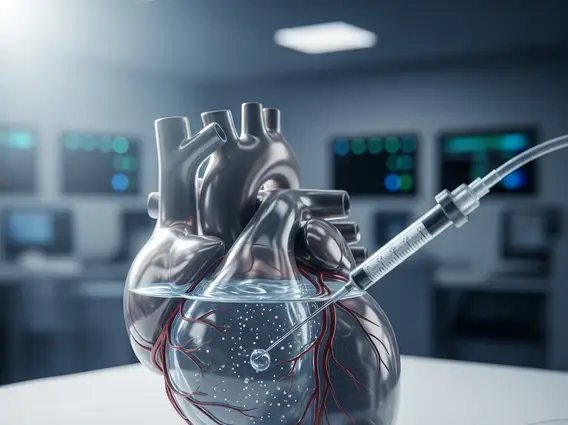
Pericardial tamponade is a critical medical condition characterized by the rapid accumulation of fluid in the pericardial sac, the double-layered membrane surrounding the heart. This fluid buildup exerts significant pressure on the heart, preventing its chambers from filling properly with blood during diastole. As a result, the heart’s ability to pump oxygenated blood to the rest of the body is severely compromised, leading to a rapid decline in circulatory function. If left untreated, it can quickly become fatal due to profound shock and cardiac arrest.
The pericardial sac normally contains a small amount of fluid that lubricates the heart and reduces friction during contractions. However, when excess fluid—such as blood, pus, or serous fluid—rapidly accumulates, the relatively inelastic nature of the pericardium means it cannot expand indefinitely. This increased pressure on the heart muscle (myocardium) and its chambers (atria and ventricles) leads to cardiac compression, directly impacting cardiac output and systemic perfusion.
Pericardial Tamponade Symptoms and Causes
Recognizing Pericardial tamponade symptoms is vital for prompt medical intervention. The clinical presentation often includes a classic triad of signs known as Beck’s triad: low arterial blood pressure, distended neck veins, and muffled heart sounds. However, patients may also experience a range of other symptoms depending on the speed of fluid accumulation and the underlying cause.
Common symptoms include:
- Severe shortness of breath (dyspnea)
- Chest pain, often sharp and radiating to the neck, shoulders, or back
- Lightheadedness or dizziness, potentially leading to fainting (syncope)
- Palpitations or a sensation of a racing heart
- Generalized weakness and fatigue
- Rapid heart rate (tachycardia)
- Cool, clammy skin, indicating poor circulation
The causes of pericardial tamponade are diverse and can stem from various medical conditions or traumatic events. The rapid accumulation of fluid, whether blood, pus, or serous fluid, is the direct trigger. According to the American Heart Association, common causes include trauma, malignancy, and inflammatory conditions affecting the pericardium.
Specific causes can include:
- Trauma: Penetrating chest injuries (e.g., stab wounds, gunshot wounds) or blunt chest trauma can cause bleeding into the pericardial sac.
- Medical Procedures: Complications from cardiac surgery, catheterizations, or pacemaker insertions can lead to pericardial effusion and subsequent tamponade.
- Malignancy: Cancers, particularly lung cancer, breast cancer, lymphoma, and melanoma, can metastasize to the pericardium, causing fluid accumulation.
- Inflammatory Conditions: Pericarditis (inflammation of the pericardium) from viral, bacterial, or autoimmune diseases (e.g., lupus, rheumatoid arthritis) can lead to effusions.
- Renal Failure: Uremic pericarditis in patients with kidney failure can cause fluid buildup.
- Myocardial Infarction: Rarely, a ruptured heart wall after a heart attack can cause blood to fill the pericardial sac.
- Aortic Dissection: A tear in the aorta can lead to blood leaking into the pericardium.
Diagnosis and Treatment for Pericardial Tamponade
Timely Pericardial tamponade diagnosis and treatment are crucial for patient survival. Diagnosis typically begins with a thorough clinical assessment, including evaluating the patient’s symptoms and physical signs like Beck’s triad and pulsus paradoxus (an abnormally large drop in blood pressure during inspiration). Rapid recognition of these signs is often the first step in identifying the condition.
Diagnostic tools commonly employed include:
- Echocardiography: This is the most definitive diagnostic test, providing real-time images of the heart and the pericardial sac. It can visualize the fluid accumulation, assess its severity, and show the compressive effects on the heart chambers, such as right ventricular collapse.
- Electrocardiogram (ECG): While not specific, ECG may show low voltage QRS complexes and electrical alternans (alternating amplitude of the QRS complexes), indicating the heart swinging in a fluid-filled sac.
- Chest X-ray: May show an enlarged cardiac silhouette if the effusion is large, often described as a “water bottle heart” appearance.
- CT Scan or MRI: Can provide more detailed images of the pericardium and surrounding structures, especially useful in identifying the cause of the effusion or ruling out other conditions.
Treatment for pericardial tamponade is an emergency and focuses on rapidly relieving the pressure on the heart. The primary intervention is pericardiocentesis, a procedure where a needle is inserted into the pericardial sac to drain the excess fluid. This is typically performed under ultrasound guidance to ensure safety and efficacy. In some cases, particularly if the fluid reaccumulates or if the underlying cause requires more extensive intervention, surgical drainage via a pericardial window or pericardiectomy may be necessary. The choice of treatment depends on the patient’s stability, the volume and type of fluid, and the underlying etiology. After the immediate life-threatening compression is relieved, addressing the root cause of the fluid accumulation is essential to prevent recurrence and manage the patient’s long-term health.
