Pericardial Effusion
Pericardial effusion is a medical condition characterized by the accumulation of excess fluid in the pericardial sac, the double-layered membrane surrounding the heart. This condition can impede the heart’s ability to pump blood effectively, leading to various symptoms and potential complications.
Key Takeaways
- Pericardial effusion involves fluid buildup around the heart, potentially impairing cardiac function.
- Symptoms range from chest pain and shortness of breath to fatigue, depending on the fluid volume and speed of accumulation.
- Causes are diverse, including infections, inflammation, trauma, and underlying medical conditions.
- Diagnosis typically involves imaging tests like echocardiography.
- Treatment options vary from watchful waiting to pericardiocentesis, aiming to relieve pressure and address the underlying cause.
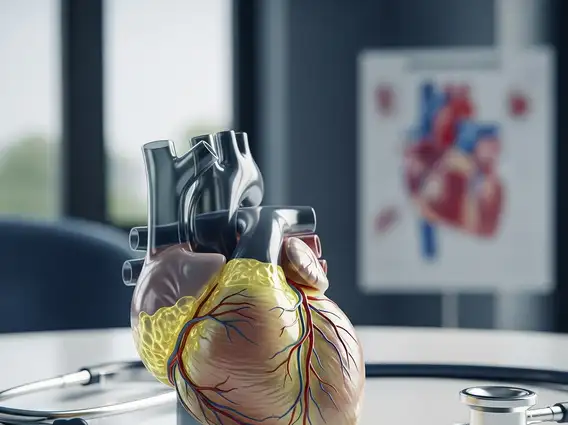
What is Pericardial Effusion?
Pericardial effusion is a condition where fluid accumulates in the pericardium, the sac that encases the heart. This sac normally contains a small amount of fluid that helps reduce friction as the heart beats. When an excessive amount of fluid builds up, it can put pressure on the heart, restricting its ability to fill with blood and pump it out effectively. The severity depends on the fluid volume and accumulation speed; rapid buildup can be more dangerous than a slow, larger accumulation.
Symptoms and Causes of Fluid Around the Heart
The pericardial effusion symptoms can vary widely depending on the amount of fluid, its accumulation speed, and the underlying cause. Mild cases may be asymptomatic. As fluid increases, pressure on the heart can lead to noticeable signs.
Common symptoms include:
- Chest pain or discomfort, often sharp and behind the breastbone, worsening with deep breathing or lying down.
- Shortness of breath (dyspnea), especially when lying flat.
- Palpitations, lightheadedness, or fainting.
- Fatigue, weakness, and swelling in the legs or abdomen.
The causes of fluid around the heart are numerous. These include:
- Infections: Viral, bacterial, fungal, or parasitic infections.
- Inflammatory Diseases: Autoimmune conditions like lupus or rheumatoid arthritis.
- Trauma: Chest injuries from accidents or medical procedures.
- Cancer: Metastatic or primary heart tumors.
- Kidney Failure: Uremia.
- Hypothyroidism: Underactive thyroid gland.
- Radiation Therapy: Radiation to the chest.
- Medications: Certain drugs as a side effect.
- Idiopathic: No specific cause identified.
Pericardial Effusion Treatment Options
The approach to pericardial effusion treatment options is highly individualized, depending on the underlying cause, effusion size, and symptom severity. Goals are to relieve pressure, address the root cause, and prevent recurrence.
For small, asymptomatic effusions, a “watch and wait” approach with regular monitoring may be adopted. If the effusion causes significant symptoms or is large, more invasive interventions may be necessary.
Common treatment strategies include:
- Medications: Anti-inflammatory drugs (NSAIDs, corticosteroids), antibiotics, antiviral medications, or diuretics.
- Pericardiocentesis: Draining excess fluid from the pericardial sac using a needle, often under ultrasound guidance. This provides immediate relief and allows fluid analysis to determine the cause.
- Pericardial Window Surgery: For recurrent effusions, a surgical opening in the pericardium allows fluid to drain into the chest cavity and be reabsorbed.
- Treatment of Underlying Condition: Addressing the primary disease, such as managing kidney failure or treating cancer, is crucial for resolution.
Prompt medical attention is vital for accurate diagnosis and appropriate management of symptoms suggestive of pericardial effusion.