Percutaneous Transhepatic Cholangiodrainage
Percutaneous Transhepatic Cholangiodrainage is a minimally invasive medical procedure used to relieve obstruction in the bile ducts. This intervention plays a crucial role in managing various conditions that lead to bile flow impairment, often providing immediate relief and improving patient outcomes.
Key Takeaways
- Percutaneous Transhepatic Cholangiodrainage (PTCD) is a minimally invasive procedure to decompress obstructed bile ducts.
- It involves inserting a catheter through the skin and liver into the bile duct under imaging guidance.
- Primary indications include malignant and benign bile duct obstructions causing jaundice or cholangitis.
- The procedure helps relieve symptoms like jaundice and can stabilize patients before definitive treatment.
- Potential risks include bleeding, infection, bile leakage, and catheter-related issues.
What is Percutaneous Transhepatic Cholangiodrainage (PTCD)?
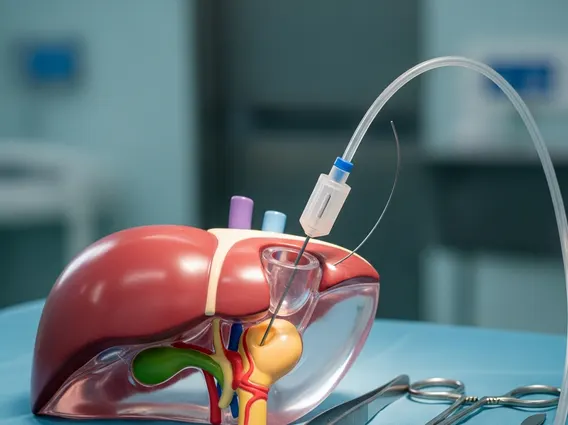
Percutaneous Transhepatic Cholangiodrainage (PTCD) is a medical procedure designed to decompress obstructed bile ducts by creating an external or internal drainage pathway. This intervention involves the percutaneous (through the skin) insertion of a catheter, guided by imaging techniques such as fluoroscopy, ultrasound, or CT, directly into the bile ducts within the liver. The primary goal is to restore bile flow, alleviate symptoms like jaundice and pruritus, and treat or prevent cholangitis, which is an infection of the bile ducts.
The procedure is typically performed by interventional radiologists and is often a temporary measure to stabilize patients before definitive surgical treatment or as a palliative solution for those with unresectable tumors. By diverting bile, PTCD helps improve liver function, reduces systemic toxicity, and can enhance the patient’s overall quality of life. Understanding what is Percutaneous Transhepatic Cholangiodrainage is crucial for patients facing bile duct obstructions, as it represents a vital therapeutic option.
Indications and Procedure for Percutaneous Transhepatic Cholangiodrainage
The Percutaneous cholangiodrainage indications are broad, primarily focusing on conditions that cause significant obstruction of the bile ducts, leading to impaired bile flow. These conditions can be malignant, such as pancreatic cancer, cholangiocarcinoma, or metastatic disease affecting the liver hilum, or benign, including gallstones, strictures from chronic pancreatitis, or iatrogenic injuries. Patients typically present with jaundice, fever, abdominal pain, or elevated liver enzymes. PTCD is often indicated when endoscopic retrograde cholangiopancreatography (ERCP) is unsuccessful or contraindicated.
The PTCD procedure explanation involves several key steps. After local anesthesia and sometimes conscious sedation, the interventional radiologist uses imaging guidance to puncture the skin and liver capsule, advancing a fine needle into an intrahepatic bile duct. Contrast material is then injected to visualize the biliary tree and identify the site of obstruction. A guidewire is threaded through the needle past the obstruction, and then a drainage catheter is advanced over the guidewire into the bile duct. The catheter can be external, draining bile into a bag outside the body, or internal-external, allowing some bile to flow into the intestine while also having an external port. The correct placement is confirmed by imaging, and the catheter is secured to the skin.
- Patient preparation and sedation.
- Imaging guidance (fluoroscopy, ultrasound, CT) to identify target bile duct.
- Percutaneous puncture of the liver and bile duct.
- Guidewire insertion past the obstruction.
- Catheter placement for drainage.
- Confirmation of catheter position and securement.
Potential Risks and Complications of PTCD
While generally safe and effective, Transhepatic bile duct drainage risks and potential complications must be considered. As with any invasive procedure, there is a risk of bleeding, which can range from minor hematoma formation at the puncture site to more significant intra-abdominal hemorrhage. Infection is another concern, including cholangitis (if not already present or exacerbated), sepsis, or local infection at the catheter insertion site. Prophylactic antibiotics are often administered to minimize this risk.
Other potential complications include bile leakage into the peritoneal cavity, which can cause peritonitis, and pneumothorax or hemothorax if the pleura is inadvertently punctured. Catheter-related issues are also common, such as dislodgement, occlusion (blockage), or breakage, requiring revision or replacement. Although rare, injury to adjacent organs like the bowel or blood vessels can occur. Patients are closely monitored post-procedure for any signs of complications, and prompt management is crucial for favorable outcomes.
