Percutaneous Ethanol Injection
Percutaneous Ethanol Injection (PEI) is a minimally invasive medical procedure utilized to treat various abnormal tissue growths, particularly certain types of tumors and cysts. This technique involves the direct injection of ethanol into the target lesion, causing cellular dehydration and protein denaturation, ultimately leading to tissue necrosis.

Key Takeaways
- Percutaneous Ethanol Injection is a minimally invasive procedure that uses ethanol to destroy abnormal tissues like tumors and cysts.
- It is guided by imaging techniques such as ultrasound or CT scans to ensure precise delivery of ethanol.
- Common uses of Percutaneous Ethanol Injection include treating small hepatocellular carcinomas, thyroid cysts, and parathyroid adenomas.
- The Percutaneous Ethanol Injection procedure is generally well-tolerated, often performed on an outpatient basis.
- While generally safe, potential Percutaneous Ethanol Injection side effects can include localized pain, fever, or temporary discomfort.
What is Percutaneous Ethanol Injection?
Percutaneous Ethanol Injection (PEI) is a therapeutic technique that involves the precise delivery of highly concentrated ethanol directly into a targeted lesion within the body. This medical procedure is considered minimally invasive, offering an alternative to more extensive surgical interventions for specific conditions. The ethanol acts as a sclerosing agent, inducing localized tissue destruction by causing cellular dehydration, protein coagulation, and infarction of small blood vessels supplying the treated area. This process effectively kills the abnormal cells while minimizing damage to surrounding healthy tissue.
PEI is often employed in oncology and endocrinology, particularly for lesions that are difficult to access surgically or for patients who may not be candidates for surgery due to other health concerns. Its efficacy and relatively low risk profile make it a valuable tool in the management of various benign and malignant conditions, providing a targeted approach to disease management.
Percutaneous Ethanol Injection Procedure and Its Uses
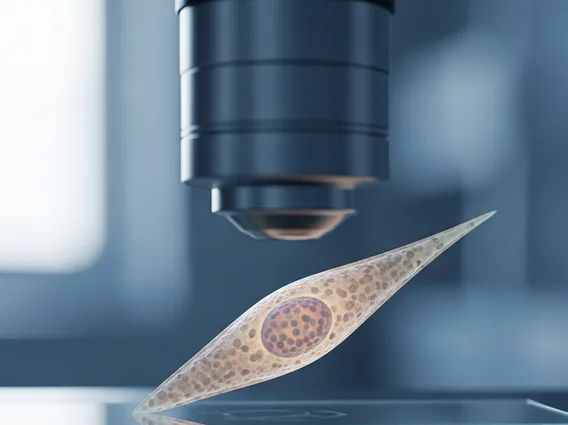
The percutaneous ethanol injection procedure typically begins with detailed imaging, such as ultrasound or computed tomography (CT) scans, to accurately locate the target lesion. Once identified, a fine needle is carefully guided through the skin and into the lesion under continuous real-time imaging guidance. This precision is crucial to ensure the ethanol is delivered directly into the abnormal tissue while avoiding adjacent vital structures. Once the needle is in place, a small amount of sterile ethanol is injected, often in multiple sessions, depending on the size and nature of the lesion.
The primary uses of percutaneous ethanol injection are diverse, ranging from the treatment of cancerous tumors to benign cysts. Some of the most common applications include:
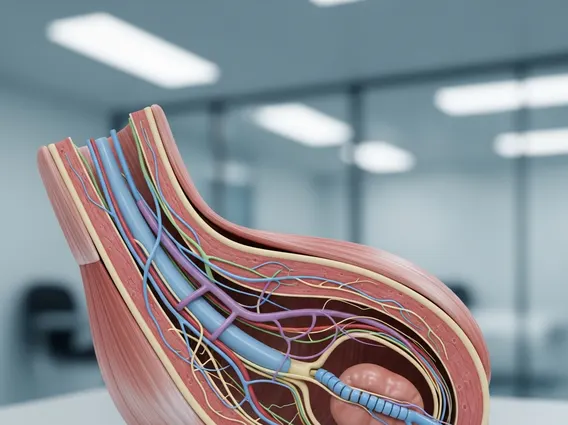
- Hepatocellular Carcinoma (HCC): PEI is particularly effective for small, early-stage liver cancers, especially in patients with underlying liver disease. Clinical studies indicate that for small HCCs (typically ≤3 cm), PEI can achieve complete tumor necrosis in a significant percentage of cases, with 5-year survival rates comparable to surgical resection in select patient groups, as reported by various medical literature.
- Thyroid Cysts and Benign Nodules: It is used to reduce the size of symptomatic benign thyroid cysts and some solid nodules, alleviating pressure symptoms and improving cosmetic appearance.
- Parathyroid Adenomas: For patients with primary hyperparathyroidism who are not surgical candidates, PEI can be used to ablate hyperfunctioning parathyroid adenomas.
- Renal Cysts: Symptomatic simple renal cysts can be treated with PEI to reduce their size and relieve associated pain or pressure.
The procedure is often performed on an outpatient basis, and patients can typically resume normal activities shortly after, though monitoring for any immediate side effects is standard.
Potential Side Effects of Percutaneous Ethanol Injection
While generally considered safe and well-tolerated, percutaneous ethanol injection side effects can occur, though they are usually mild and temporary. The most common side effects are related to the injection site and the immediate effects of ethanol on surrounding tissues. Patients may experience localized pain or discomfort at the injection site, which can often be managed with over-the-counter pain relievers. A low-grade fever, nausea, or a general feeling of malaise can also occur temporarily after the procedure.
Less common but more serious complications can include bleeding or hematoma formation, infection at the injection site, or damage to adjacent organs or structures if the ethanol spreads beyond the target lesion. For liver treatments, transient elevation of liver enzymes or a temporary worsening of liver function can sometimes be observed. However, with precise imaging guidance and careful technique, the risk of severe complications is minimized. Patients are typically monitored post-procedure to ensure any potential side effects are promptly addressed.