Pd 1
This article explores Programmed Cell Death Protein 1 (PD-1), a crucial component of the immune system, and its significant role in regulating immune responses. Understanding PD-1 is vital for comprehending its implications in various diseases, particularly cancer.
Key Takeaways
- PD-1 is a protein on immune cells that helps prevent them from attacking healthy cells.
- It acts as an immune checkpoint, signaling T-cells to stand down when it binds to its ligands.
- Dysregulation of the PD-1 pathway can allow cancer cells to evade immune detection and destruction.
- PD-1 inhibitors are a class of drugs that block this pathway, reactivating the immune system against tumors.
- These inhibitors have revolutionized cancer treatment by harnessing the body’s natural defenses.
What is PD-1 (Programmed Cell Death Protein 1)?
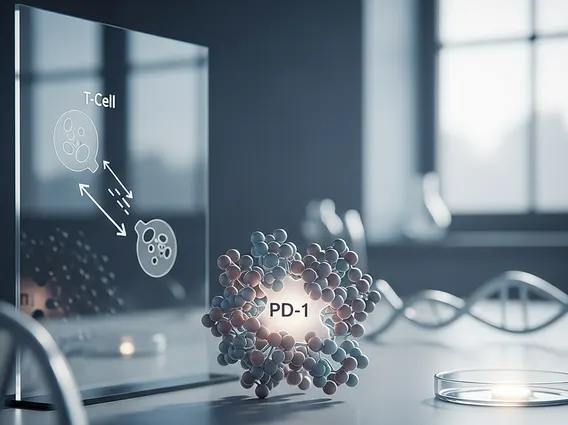
PD-1 (Programmed Cell Death Protein 1) is a cell surface receptor found on T-cells, a type of white blood cell critical to the immune system. It belongs to the CD28 superfamily of immune checkpoint receptors. Its primary role is to regulate the immune response by preventing excessive immune activity that could harm healthy tissues. Essentially, PD-1 acts as an “off switch” for T-cells, ensuring immune tolerance and preventing autoimmune diseases.
When PD-1 binds to its ligands, PD-L1 (Programmed Death-Ligand 1) or PD-L2 (Programmed Death-Ligand 2), it sends inhibitory signals to the T-cell. This interaction suppresses T-cell activation, proliferation, and cytokine production, effectively dampening the immune response. This mechanism is crucial for maintaining a balanced immune system, but it can be exploited by cancer cells.
PD-1 Protein Function and Pathway Explained
The PD-1 protein function is central to immune regulation. It acts as an immune checkpoint, a molecular brake that prevents the immune system from overreacting. This function is particularly important in peripheral tissues, where T-cells might encounter self-antigens. By engaging PD-1, these T-cells are inhibited, thus preventing autoimmune reactions. The ligands for PD-1, primarily PD-L1 and PD-L2, are expressed on various cell types, including antigen-presenting cells, and can be upregulated in response to inflammation or infection.
The PD-1 pathway explained involves the interaction between the PD-1 receptor on T-cells and its ligands. When a T-cell recognizes an antigen, it becomes activated. However, if that T-cell also encounters a cell expressing PD-L1 or PD-L2, the binding of these ligands to PD-1 triggers an inhibitory cascade within the T-cell. This cascade leads to reduced T-cell activation, decreased cytokine release (such as interferon-gamma and TNF-alpha), and often, T-cell exhaustion or apoptosis. Many cancer cells exploit this natural pathway by overexpressing PD-L1 on their surface, effectively creating an immune-suppressive microenvironment that allows them to evade destruction by the immune system.
Key components of the PD-1 pathway include:
- PD-1 Receptor: Found on activated T-cells, B-cells, NK cells, and myeloid cells.
- PD-L1 Ligand: Widely expressed on immune cells, tumor cells, and other tissues; often upregulated in inflammatory conditions and cancers.
- PD-L2 Ligand: More restricted expression, primarily on antigen-presenting cells.
- Signaling Cascade: Binding of PD-1 to its ligands activates phosphatases that dephosphorylate key signaling molecules, inhibiting T-cell activation.
Mechanism of PD-1 Inhibitors
The PD-1 inhibitors mechanism involves blocking the interaction between the PD-1 receptor and its ligands, PD-L1 and PD-L2. These inhibitors are a class of immunotherapeutic drugs, often monoclonal antibodies, designed to disrupt this immune checkpoint. By preventing PD-1 from binding to its ligands, these drugs effectively “release the brakes” on the T-cells, allowing them to reactivate and mount an effective immune response against cancer cells.
When a PD-1 inhibitor binds to the PD-1 receptor on a T-cell, it physically blocks PD-L1 and PD-L2 from attaching. This blockade prevents the inhibitory signals that would normally suppress the T-cell. As a result, the T-cell remains active, capable of recognizing and destroying cancer cells that might be expressing PD-L1. This approach has revolutionized cancer treatment, particularly for melanoma, non-small cell lung cancer, renal cell carcinoma, and other malignancies, by harnessing the patient’s own immune system to fight the disease.
