Paterson Kelly Syndrome
Paterson Kelly Syndrome, also known as Plummer-Vinson Syndrome, is a rare disorder characterized by a classic triad of symptoms affecting the upper gastrointestinal tract. This article provides a detailed overview of its presentation, underlying factors, and management strategies.
Key Takeaways
- Paterson Kelly Syndrome is a rare condition involving esophageal webs, iron-deficiency anemia, and often difficulty swallowing.
- The primary cause is strongly linked to chronic iron deficiency, though genetic and autoimmune factors may also contribute.
- Common symptoms include dysphagia, fatigue, and signs of anemia like pallor and brittle nails.
- Diagnosis typically involves endoscopy and blood tests, with treatment focused on iron supplementation and web dilation.
- With appropriate management, the prognosis is generally favorable, but long-term monitoring is advised due to a slightly increased risk of post-cricoid esophageal cancer.
What is Paterson Kelly Syndrome?
Paterson Kelly Syndrome is a rare condition defined by the presence of esophageal webs, iron-deficiency anemia, and dysphagia (difficulty swallowing). It is also widely recognized by its alternative name, Plummer-Vinson Syndrome. This syndrome primarily affects the upper esophagus, where thin membranes of tissue, known as esophageal webs, can form, partially obstructing the passage of food. While historically more prevalent, its incidence has significantly declined in developed countries due to improved nutritional intake and early treatment of iron deficiency, making it a truly uncommon diagnosis today.
Beyond the characteristic esophageal webs and iron-deficiency anemia, individuals with this syndrome may also experience other symptoms related to chronic iron deficiency, such as glossitis (inflammation of the tongue), angular stomatitis (fissures at the corners of the mouth), and koilonychia (spoon-shaped nails). The exact mechanism by which iron deficiency leads to web formation is not fully understood, but it is thought to involve impaired regeneration of epithelial cells in the pharynx and esophagus.
Symptoms, Causes, and Risk Factors
Understanding the presentation of this condition is crucial for early detection. The primary indicators of Paterson Kelly Syndrome symptoms causes often revolve around the difficulty in swallowing and the systemic effects of anemia. The most prominent symptom is dysphagia, which typically begins with solid foods and may progress to liquids. This difficulty is caused by the esophageal webs physically narrowing the food pipe.
Other common symptoms include:
- Fatigue and Weakness: Direct results of iron-deficiency anemia, impacting energy levels and overall physical stamina.
- Pallor: A noticeable paleness of the skin and mucous membranes due to reduced red blood cell count.
- Glossitis: A smooth, red, and often painful tongue, indicative of nutritional deficiencies.
- Angular Cheilitis: Cracks or sores at the corners of the mouth, also linked to iron deficiency.
- Koilonychia: Brittle, spoon-shaped fingernails, a classic sign of chronic iron deficiency.
The exact cause of Paterson Kelly Syndrome remains elusive, but it is strongly associated with chronic iron deficiency. While the direct link is clear, the specific mechanism by which iron deficiency leads to esophageal web formation is not fully understood. Some theories suggest that iron deficiency impairs the regenerative capacity of the esophageal mucosa, making it more susceptible to damage and web formation. Risk factors include being female, particularly middle-aged women, and individuals with poor nutritional status or conditions leading to chronic blood loss or malabsorption, such as celiac disease or inflammatory bowel disease. Genetic predisposition and autoimmune factors have also been considered as potential contributing elements.
Diagnosis, Treatment, and Outlook
The identification and management of this rare syndrome require a careful approach. Paterson Kelly Syndrome diagnosis treatment typically begins with a thorough medical history and physical examination, focusing on symptoms like dysphagia and signs of anemia. Blood tests are essential to confirm iron-deficiency anemia, including a complete blood count (CBC) to check hemoglobin levels and iron studies (serum iron, ferritin, total iron-binding capacity).
The definitive diagnosis of esophageal webs is usually made through:
- Barium Swallow: An imaging test where the patient swallows a barium solution, allowing X-rays to visualize the esophagus and detect any obstructions or webs.
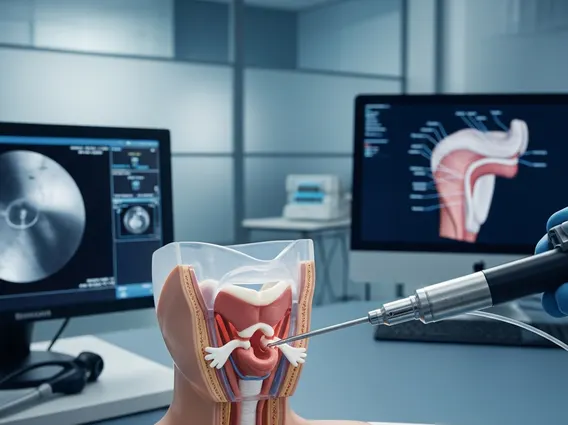
- Upper Endoscopy: A procedure where a thin, flexible tube with a camera is inserted down the throat to directly visualize the esophageal lining and identify webs. This also allows for biopsies if needed to rule out other conditions.
Treatment primarily focuses on two key aspects: correcting the iron deficiency and addressing the esophageal webs. Iron supplementation, either oral or intravenous, is crucial to resolve the anemia and prevent the recurrence of webs. For the dysphagia caused by the webs, endoscopic dilation is often performed. During this procedure, a balloon or dilator is used to gently stretch and break the web, restoring the normal passage for food. With proper treatment, the immediate relief from dysphagia is usually significant.
The Paterson Kelly Syndrome prognosis is generally good with appropriate and timely treatment. Most individuals experience a complete resolution of symptoms once iron levels are normalized and esophageal webs are dilated. However, due to a slightly increased, though still rare, risk of developing post-cricoid esophageal cancer, long-term follow-up and regular monitoring are often recommended. This emphasizes the importance of continued medical care to ensure sustained health and early detection of any potential complications.
