Pap
The term Pap, in a medical context, most commonly refers to the Papanicolaou test, a vital screening tool for cervical health. This article explores the significance of this test in preventing cervical cancer.
Key Takeaways
- The Pap test is a crucial screening method for detecting abnormal cells on the cervix.
- Regular Pap tests are essential for the early detection and prevention of cervical cancer, often caused by HPV.
- The procedure involves collecting cervical cells for microscopic examination.
- Understanding your Pap test results helps guide necessary follow-up care, even if results are abnormal.
- Routine screening significantly reduces cervical cancer incidence and mortality.
What is a Pap Test (Pap Smear)?
A Pap test, also known as a Pap smear, is a gynecological screening procedure designed to detect precancerous or cancerous cells on the cervix. The cervix is the lower, narrow end of the uterus that opens into the vagina. This test plays a critical role in women’s health by identifying cellular changes that, if left untreated, could potentially develop into cervical cancer. The primary goal of a Pap test is early detection, allowing for timely intervention and significantly improving treatment outcomes. The effectiveness of the Pap test in reducing cervical cancer mortality is well-documented; for instance, the Centers for Disease Control and Prevention (CDC) highlights that regular screening can prevent most cases of cervical cancer.
Why Get a Pap Test? The Procedure Explained
Regular Pap tests are a cornerstone of preventive healthcare for women, primarily because they are highly effective in preventing cervical cancer. Cervical cancer is often caused by persistent infection with certain types of human papillomavirus (HPV), a common sexually transmitted infection. By detecting abnormal cells early, before they become cancerous, a Pap test allows for prompt treatment, thereby preventing the progression of the disease. According to the World Health Organization (WHO), cervical cancer is largely preventable through vaccination against HPV and screening programs like the Pap test.
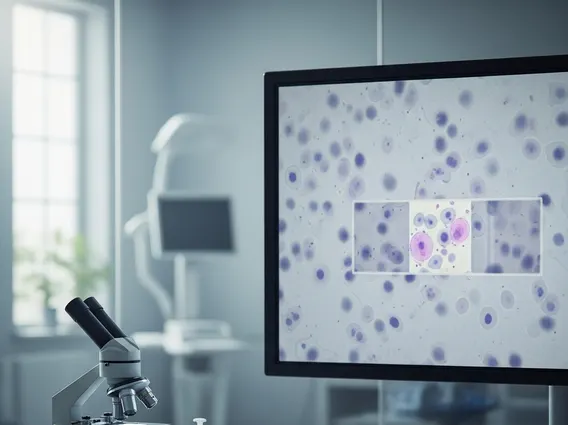
The pap smear procedure is typically performed during a routine pelvic exam and is generally quick, causing minimal discomfort. During the test, your healthcare provider will use a speculum to gently open the vaginal walls, allowing visualization of the cervix. A small brush or spatula is then used to collect cells from the cervix. These cells are immediately preserved and sent to a lab for analysis.
To ensure the most accurate results, it is often recommended to follow a few guidelines before your Pap test:
- Avoid douching, using vaginal medicines, or spermicidal products for at least 24-48 hours before the test.
- Refrain from sexual intercourse for 24-48 hours prior to the test.
- Schedule your test for a time when you are not menstruating, as blood can interfere with the results.
These steps help ensure that collected cervical cells are clear and free from potential contaminants, allowing for a more accurate assessment.
Understanding Your Pap Test Results
Receiving and understanding pap test results is a crucial step in managing your cervical health. After your Pap test, it typically takes a few days to a couple of weeks to get the results back from the laboratory. Results are generally categorized as normal (negative) or abnormal (positive). A normal result means that no abnormal cells were found, and you can usually continue with routine screening as recommended by your doctor, often every three years for women aged 21-65.
An abnormal Pap test result does not automatically mean you have cancer. Instead, it indicates that some cells on your cervix appear unusual and require further investigation. Abnormal results can range from minor changes to more significant ones. Common abnormal findings include:
- Atypical Squamous Cells of Undetermined Significance (ASCUS): Mild changes, often due to inflammation or HPV infection.
- Low-Grade Squamous Intraepithelial Lesion (LSIL): Mildly abnormal changes, usually caused by HPV infection.
- High-Grade Squamous Intraepithelial Lesion (HSIL): More significant precancerous changes with a higher chance of progressing to cancer if untreated.
- Atypical Glandular Cells (AGC): Abnormal cells found in the glandular tissue of the cervix or uterus.
Depending on the type and severity of the abnormal cells, your healthcare provider may recommend additional tests, such as an HPV test, a colposcopy (a magnified examination of the cervix), or a biopsy. These follow-up procedures help determine the exact cause of the abnormalities and guide appropriate treatment. Regular follow-up is key to managing any detected changes effectively.