Palliative Sedation
Palliative Sedation is a medical intervention aimed at alleviating intractable suffering in patients nearing the end of life when all other palliative measures have failed. It involves the controlled administration of sedative medications to reduce consciousness, providing comfort and peace during a patient’s final days.
Key Takeaways
- Palliative Sedation is a medical practice to relieve severe, refractory suffering in terminally ill patients.
- Its primary palliative sedation purpose is to manage symptoms unresponsive to conventional treatments, not to hasten death.
- The process involves careful assessment, informed consent, and continuous monitoring of medication administration.
- Significant palliative sedation ethical considerations include patient autonomy, the distinction from euthanasia, and proportionality of sedation.
- It requires a multidisciplinary team approach to ensure patient comfort and dignity.
What is Palliative Sedation?
Palliative Sedation refers to the use of sedative medications to induce a state of decreased or absent awareness in a patient who is experiencing severe and intractable suffering at the end of life. This medical intervention is considered when all other conventional treatments and palliative care strategies have failed to adequately control distressing symptoms such as pain, dyspnea (shortness of breath), delirium, or existential distress. The goal is to provide relief from suffering, not to intentionally shorten life, distinguishing it clearly from euthanasia or physician-assisted suicide. It is a last-resresort measure, implemented only after thorough evaluation and discussion with the patient and their family.
Purpose and Process of Palliative Sedation
The primary palliative sedation purpose is to alleviate refractory symptoms that cause unbearable suffering for a patient with a terminal illness. These symptoms are considered “refractory” when they are resistant to all appropriate and aggressive conventional treatments, including specialized palliative care interventions. The intent is solely to provide comfort and dignity in the final stages of life, allowing the patient to experience a peaceful passing.
How Does Palliative Sedation Work?
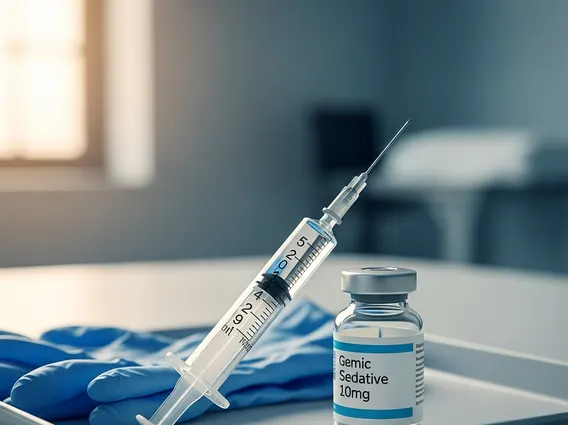
The process of Palliative Sedation involves several critical steps, beginning with a comprehensive assessment by a multidisciplinary team. This team typically includes physicians, nurses, social workers, and chaplains, who confirm the refractory nature of the symptoms and ensure all other options have been exhausted. Informed consent is paramount; the patient, if capable, or their legally authorized surrogate, must fully understand the goals, benefits, and potential risks of sedation. Medications such as midazolam, propofol, or phenobarbital are commonly used, administered incrementally to achieve the desired level of sedation, which can range from light (drowsiness) to deep (unconsciousness). The patient’s vital signs and comfort levels are continuously monitored, and medication dosages are adjusted to maintain symptom control while avoiding over-sedation beyond what is necessary for relief.
Ethical Considerations for Palliative Sedation
The implementation of Palliative Sedation involves complex palliative sedation ethical considerations that require careful navigation by healthcare providers, patients, and their families. These considerations ensure that the practice remains patient-centered, compassionate, and ethically sound. Key ethical points include:
- Patient Autonomy and Informed Consent: Ensuring the patient’s wishes are respected, either directly or through advance directives and surrogate decision-makers. Consent must be fully informed, understanding the nature and implications of sedation.
- Distinction from Euthanasia: Clearly differentiating Palliative Sedation, where the intent is to relieve suffering, from euthanasia, which aims to intentionally end life. The ethical framework emphasizes that Palliative Sedation does not hasten death.
- Proportionality of Sedation: Administering the minimum effective dose of sedatives required to achieve symptom relief, avoiding excessive sedation that is not medically necessary.
- Refractory Symptoms: Rigorously confirming that symptoms are genuinely refractory and that all other reasonable palliative interventions have been attempted and failed.
- Impact on Family and Caregivers: Providing comprehensive support and clear communication to family members, addressing their concerns and grief throughout the process.
- Multidisciplinary Review: Encouraging a team-based approach involving various healthcare professionals to ensure a thorough ethical review and consensus on the decision to initiate Palliative Sedation.
