Ophthalmoscopy
Ophthalmoscopy, also known as fundoscopy, is a crucial diagnostic procedure used by eye care professionals to examine the internal structures of the eye, particularly the retina, optic disc, macula, and vitreous humor. This examination provides vital insights into eye health and can detect various systemic diseases.
Key Takeaways
- Ophthalmoscopy is an eye examination that allows a doctor to look at the back of the eye (fundus).
- It is performed using specialized instruments like an ophthalmoscope, often after pupil dilation.
- The purpose of ophthalmoscopy is to detect and monitor eye diseases such as glaucoma, diabetic retinopathy, and macular degeneration.
- Common types of ophthalmoscopy include direct, indirect, and slit-lamp fundoscopy, each offering different views and magnifications.
- Regular ophthalmoscopic examinations are essential for early detection and management of conditions affecting vision and overall health.
What is Ophthalmoscopy?
Ophthalmoscopy is a non-invasive diagnostic procedure that enables a healthcare provider to visualize the fundus, or the back part of the eye. This includes the retina, optic disc, macula, and choroid. By examining these structures, clinicians can identify signs of various ocular diseases and systemic conditions that manifest in the eye. It is a fundamental component of a comprehensive eye examination, offering a direct view of the blood vessels, nerve tissue, and other critical components at the back of the eye.
This examination is essential for assessing the health of the optic nerve, which transmits visual information from the eye to the brain, and the retina, the light-sensitive tissue responsible for vision. Early detection of abnormalities through ophthalmoscopy can lead to timely intervention and potentially prevent severe vision loss.
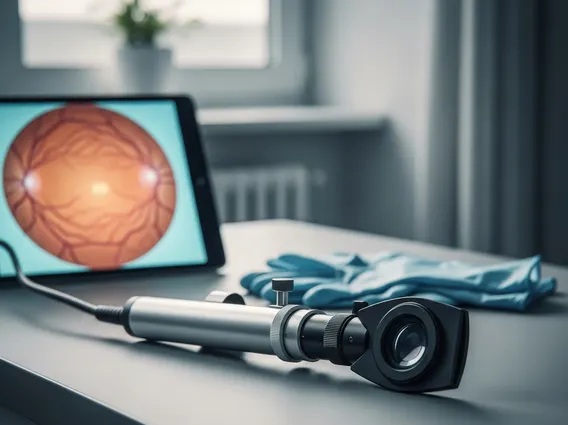
How is Ophthalmoscopy Performed?
The procedure for how is ophthalmoscopy performed typically involves the use of an ophthalmoscope, a specialized instrument that shines a light into the eye and allows the examiner to view the internal structures. Before the examination, eye drops may be administered to dilate the pupils, which widens them to provide a clearer and broader view of the fundus. This dilation usually takes about 15-30 minutes to take effect and can cause temporary light sensitivity and blurred vision.
During the examination, the patient is usually seated in a darkened room. The ophthalmologist or optometrist will hold the ophthalmoscope close to the patient’s eye and shine a beam of light through the pupil. The patient will be asked to look in different directions to allow the examiner to view various parts of the retina. The process is generally quick and painless, though some patients may experience mild discomfort from the bright light. The specific technique can vary depending on the type of ophthalmoscopy being performed.
- Pupil Dilation: Eye drops are applied to enlarge the pupils, enhancing visibility of the fundus.
- Darkened Room: The examination takes place in dim lighting to optimize contrast and visibility.
- Instrument Use: The clinician uses an ophthalmoscope to direct light into the eye and observe the internal structures.
- Patient Cooperation: The patient is asked to gaze in specific directions to facilitate a comprehensive view of the retina and optic nerve.
Purpose and Types of Ophthalmoscopy
The primary purpose of ophthalmoscopy is to diagnose and monitor a wide range of eye conditions and systemic diseases. It is invaluable for detecting signs of glaucoma, diabetic retinopathy, macular degeneration, retinal detachment, and optic nerve damage. Beyond ocular conditions, ophthalmoscopy can reveal indications of systemic issues such as hypertension, stroke, and brain tumors, as the blood vessels and nerve tissue in the retina are often affected by these conditions. For instance, according to the Centers for Disease Control and Prevention (CDC), diabetic retinopathy, a condition often detected through ophthalmoscopy, affects an estimated 8.0 million adults aged 18 years or older in the United States.
There are several types of ophthalmoscopy, each offering distinct advantages:
Direct Ophthalmoscopy: This method uses a handheld instrument to provide an upright, magnified view (approximately 15 times) of a small area of the fundus. It is excellent for detailed examination of the optic disc and macula and is commonly used in routine eye exams.
Indirect Ophthalmoscopy: This technique uses a bright light source worn on the examiner’s head and a handheld condensing lens. It provides a wider, less magnified (2-5 times) but stereoscopic (3D) view of the retina, allowing for a more comprehensive assessment of the peripheral retina. This is particularly useful for detecting conditions like retinal tears or detachments.
Slit-Lamp Fundoscopy (or Biomicroscopy with Fundus Lens): This method combines a slit lamp microscope with a special handheld lens. It offers a highly magnified, stereoscopic view of the fundus, allowing for extremely detailed examination of specific areas. It is often preferred for precise evaluation of the optic nerve head, macula, and vitreous.