Neurofibroma
Neurofibroma is a common type of benign nerve sheath tumor that can develop anywhere in the nervous system. While typically non-cancerous, these growths can sometimes cause a range of symptoms depending on their size and location.
Key Takeaways
- Neurofibroma is a benign tumor originating from nerve sheaths, often associated with neurofibromatosis type 1 (NF1).
- Symptoms vary widely based on the tumor’s size and location, ranging from skin bumps to pain or neurological issues.
- Diagnosis involves physical examination, imaging (MRI, CT), and sometimes biopsy.
- Treatment options include watchful waiting, surgical removal, and targeted therapies for specific types.
- While generally benign, monitoring is crucial due to potential complications and rare malignant transformation.
What is Neurofibroma?
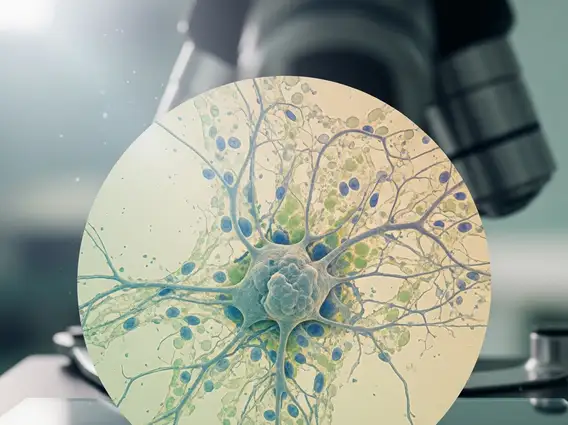
Neurofibroma refers to a type of benign (non-cancerous) tumor that develops on nerve tissue. These tumors originate from Schwann cells, which form the myelin sheath around nerves, and fibroblasts, which are connective tissue cells. They can occur anywhere in the body where there are nerves, including under the skin, along major nerves, or within internal organs. While often solitary, multiple neurofibromas are a hallmark feature of neurofibromatosis type 1 (NF1), a genetic disorder. These tumors typically grow slowly and are generally not life-threatening, but their location and size can lead to various symptoms and complications.
Neurofibroma Symptoms, Causes, and Diagnosis
The presentation of neurofibromas can vary significantly, making neurofibroma symptoms and causes a broad topic. Symptoms largely depend on the tumor’s location and size. Many neurofibromas, especially those located superficially under the skin, may be asymptomatic, presenting only as soft, flesh-colored bumps. However, if a neurofibroma grows on a nerve or presses against surrounding tissues, it can cause pain, numbness, tingling, or weakness in the affected area. Internal neurofibromas might lead to organ dysfunction. The primary cause of multiple neurofibromas is a genetic mutation in the NF1 gene, which regulates cell growth. Solitary neurofibromas, however, often occur sporadically without a clear genetic link.
Diagnosing neurofibroma typically begins with a thorough physical examination and a review of the patient’s medical history. A doctor will look for characteristic skin findings, such as café-au-lait spots or freckling, common in NF1. Imaging studies are crucial for confirming the presence and extent of neurofibromas, especially those not visible on the skin.
- Magnetic Resonance Imaging (MRI): Preferred for visualizing nerve tumors in the brain, spinal cord, or deep tissues.
- Computed Tomography (CT) Scan): Used to identify tumors and assess their impact on bone structures.
- Biopsy: A tissue sample may be taken to confirm diagnosis and rule out malignancy, particularly with rapid growth or unusual features.
Genetic testing can also confirm an NF1 diagnosis, especially in individuals with a family history or multiple characteristic features.
Neurofibroma Treatment Options
The approach to neurofibroma treatment options is highly individualized, depending on the tumor’s size, location, symptoms, and association with conditions like NF1. For many asymptomatic neurofibromas, a “watch and wait” approach is often recommended, involving regular monitoring.
When treatment is necessary, surgical removal is the most common and effective option, especially for solitary, symptomatic, or rapidly growing tumors. The goal is to remove as much of the tumor as possible while preserving nerve function. Complete removal can be challenging if the tumor is deeply intertwined with a nerve, carrying a risk of nerve damage.
Other treatment modalities may include:
- Pain Management: For neurofibromas causing chronic pain, various strategies like medication or nerve blocks may be employed.
- Targeted Therapy: For extensive plexiform neurofibromas associated with NF1, targeted therapies such as MEK inhibitors (e.g., selumetinib) have shown promise in shrinking tumors and improving symptoms. These are typically reserved for cases causing significant morbidity.
- Radiation Therapy: Rarely used for benign neurofibromas due to potential side effects and the risk of inducing malignant transformation, it may be considered in specific, complex cases where surgery is not feasible.
Individuals with neurofibromas, particularly those with NF1, should have regular follow-ups with a multidisciplinary team of specialists to manage their condition comprehensively and monitor for complications or malignant changes.
