Neuroendocrine Carcinoma Of The Skin
Neuroendocrine Carcinoma Of The Skin is a rare and aggressive form of skin cancer that originates from neuroendocrine cells in the skin. This article provides a comprehensive overview of this condition, including its characteristics, symptoms, diagnostic methods, causes, and available treatment options.
Key Takeaways
- Neuroendocrine Carcinoma Of The Skin, also known as Merkel cell carcinoma, is a rare and highly aggressive skin cancer.
- It typically presents as a rapidly growing, painless nodule, often in sun-exposed areas.
- Diagnosis relies on biopsy and pathological examination, with early detection being crucial due to its aggressive nature.
- The primary cause is often the Merkel cell polyomavirus (MCPyV), particularly in individuals with weakened immune systems.
- Treatment usually involves a multidisciplinary approach, including surgery, radiation, and systemic therapies like immunotherapy.
What Is Neuroendocrine Carcinoma Of The Skin?
Neuroendocrine Carcinoma Of The Skin refers to a rare and highly aggressive type of skin cancer that develops from neuroendocrine cells located in the skin. These cells are found in the top layer of the skin and have characteristics of both nerve cells and hormone-producing cells. This malignancy is more commonly known as Merkel cell carcinoma (MCC) and is distinguished by its rapid growth and high potential for metastasis to lymph nodes and distant organs. While relatively uncommon, with an estimated incidence of less than 1 per 100,000 people in the United States, according to the American Cancer Society, its aggressive nature makes early detection and treatment critical.
The exact function of normal Merkel cells is not fully understood, but they are thought to play a role in touch sensation. When these cells become cancerous, they form tumors that can appear anywhere on the body, though they are most frequently found on sun-exposed areas such as the head, neck, arms, and legs. Understanding what is neuroendocrine carcinoma of the skin involves recognizing its cellular origin and its propensity for rapid progression.
Symptoms and Diagnosis of Neuroendocrine Skin Tumors
Recognizing Neuroendocrine carcinoma skin symptoms is crucial for timely intervention. This type of tumor often presents as a single, rapidly growing, firm, painless, and shiny nodule on the skin. The color can range from red to purple or skin-colored. Due to its often innocuous appearance and lack of pain in early stages, it can sometimes be mistaken for a benign cyst or other common skin lesion, leading to delays in diagnosis. However, its characteristic rapid growth should always prompt medical evaluation.
Common symptoms and characteristics include:
- A rapidly enlarging, firm, dome-shaped nodule.
- Painless lesion, which can sometimes lead to delayed presentation.
- Often found on sun-exposed areas like the face, neck, or limbs.
- May appear red, purple, or skin-colored.
- Can sometimes ulcerate or bleed in later stages.
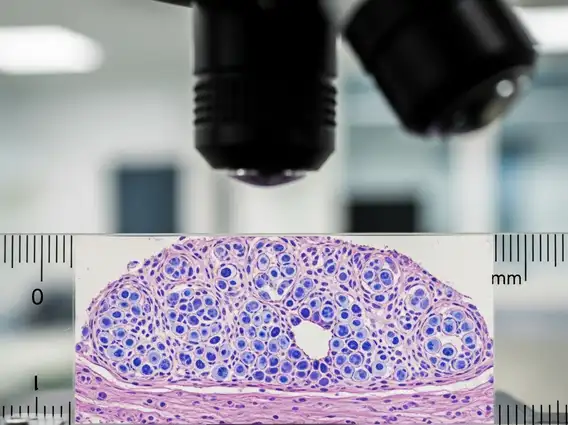
The definitive Skin neuroendocrine tumor diagnosis typically begins with a thorough clinical examination, followed by a biopsy of the suspicious lesion. A punch biopsy or excisional biopsy is usually performed, and the tissue sample is then examined by a pathologist under a microscope. Immunohistochemical staining is a critical part of the diagnostic process, as it helps identify specific markers (e.g., cytokeratin 20, neurofilament) that confirm the neuroendocrine origin of the tumor cells. Imaging tests, such as CT scans, PET scans, or MRI, are often used to determine the extent of the disease and check for metastasis to lymph nodes or other organs, which is vital for staging and treatment planning.
Causes and Treatment for Merkel Cell Carcinoma
The primary cause of Merkel cell carcinoma causes and treatment is strongly linked to infection with the Merkel cell polyomavirus (MCPyV). This virus is found in about 80% of MCC tumors. While many people are exposed to MCPyV, only a small fraction develop MCC, suggesting that other factors contribute to its development. Immunosuppression, whether due to medical conditions like HIV/AIDS, organ transplantation, or certain autoimmune diseases, significantly increases the risk. Chronic exposure to ultraviolet (UV) radiation from sunlight is also considered a significant risk factor, as many tumors develop on sun-exposed skin.
Treatment for Merkel cell carcinoma is typically aggressive and multidisciplinary, tailored to the stage and extent of the disease. The main treatment modalities include:
- Surgery: Often the first line of treatment, involving wide local excision of the tumor. Sentinel lymph node biopsy is frequently performed to check for spread to nearby lymph nodes.
- Radiation Therapy: Commonly used after surgery to destroy any remaining cancer cells in the tumor bed or regional lymph nodes, and sometimes as a primary treatment for unresectable tumors.
- Systemic Therapy: For advanced or metastatic disease, immunotherapy (e.g., with PD-1 inhibitors like pembrolizumab or avelumab) has shown significant promise. Chemotherapy may also be used, though it is often reserved for cases where immunotherapy is not effective or appropriate.
Given the aggressive nature of MCC, a combination of these treatments is often necessary to achieve the best possible outcomes. Regular follow-up is essential to monitor for recurrence, as MCC has a high rate of local recurrence and distant metastasis.
