Nerve Sparing Surgery
Nerve Sparing Surgery is a specialized surgical technique designed to preserve nerve function during the removal of diseased tissue or organs. This advanced approach aims to minimize post-operative complications such as incontinence or erectile dysfunction, significantly improving patients’ quality of life.
Key Takeaways
- Nerve Sparing Surgery is a specialized technique focused on preserving critical nerves during tumor removal.
- It is commonly applied in prostatectomy, hysterectomy, and colorectal surgeries to reduce functional side effects.
- The procedure involves meticulous identification and careful dissection around nerve bundles.
- Benefits include a lower risk of urinary incontinence, erectile dysfunction, and improved quality of life.
- Recovery focuses on managing pain, monitoring nerve function, and gradual return to activity.
What is Nerve Sparing Surgery?
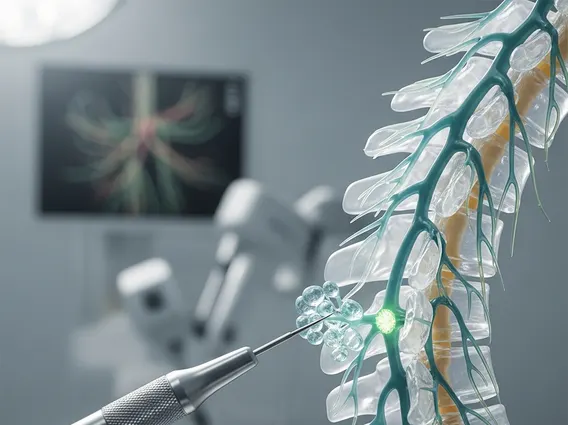
Nerve Sparing Surgery refers to a sophisticated surgical technique employed to remove cancerous or diseased tissue while meticulously preserving adjacent nerves critical for bodily functions. The primary goal of this procedure is to reduce the risk of common post-operative complications that arise from nerve damage, such as urinary incontinence, sexual dysfunction, or bowel control issues. This approach is particularly vital in areas where nerves are closely intertwined with the target organ, such as the prostate, rectum, or uterus. By carefully identifying and protecting these delicate nerve bundles, surgeons aim to maintain the patient’s quality of life following the primary surgical intervention. The efficacy of nerve sparing surgery depends heavily on the surgeon’s skill, anatomical knowledge, and the extent of the disease.
The Surgical Procedure for Nerve Sparing
The nerve sparing surgery procedure involves a highly detailed and precise approach to surgical dissection. Before the operation, advanced imaging techniques, such as MRI, are often used to map the anatomy and the proximity of nerves to the diseased area. During the surgery, the surgeon uses specialized instruments and magnification to carefully separate the nerve bundles from the tissue being removed. This often requires a slower, more deliberate pace compared to conventional surgery. For instance, in a radical prostatectomy, the neurovascular bundles responsible for erectile function are identified and carefully dissected away from the prostate gland. The exact steps can vary significantly depending on the specific organ and the location of the disease.
Key steps often include:
- Pre-operative Imaging: Detailed scans to visualize nerve pathways and tumor margins.
- Careful Incision and Exposure: Accessing the surgical site with minimal disruption to surrounding tissues.
- Nerve Identification: Using visual cues, and sometimes nerve stimulation, to locate critical nerve bundles.
- Meticulous Dissection: Gently separating nerves from the diseased organ or tissue using fine instruments.
- Tissue Removal: Excising the target tissue while ensuring nerve integrity.
- Reconstruction (if necessary): Repairing or reconstructing tissues as required.
This intricate process demands exceptional surgical precision and a deep understanding of neuroanatomy to achieve optimal outcomes.
Benefits and Post-Operative Recovery
The benefits of nerve sparing surgery are significant, primarily revolving around the preservation of crucial bodily functions and an improved quality of life for patients. By minimizing damage to nerves, patients experience a lower incidence and severity of common post-operative complications. For example, in prostate cancer surgery, nerve sparing techniques have been shown to significantly improve rates of urinary continence and erectile function compared to non-nerve sparing approaches. This leads to better long-term functional outcomes and overall patient satisfaction.
Recovery after nerve sparing surgery typically involves a period of healing and rehabilitation, which can vary based on the type of surgery and individual patient factors. Immediately after the procedure, pain management is a priority. Patients are closely monitored for any signs of nerve dysfunction or other complications. While the goal is to preserve nerve function, some temporary impairment or delayed recovery of function can occur as nerves heal. Rehabilitation might include pelvic floor exercises for urinary continence or specific therapies to aid in the return of sexual function. Most patients are encouraged to gradually increase their activity levels, with full recovery often taking several weeks to months. Regular follow-up appointments with the surgical team are essential to monitor progress and address any ongoing concerns, ensuring the best possible long-term outcomes.
