Naxitamab
Naxitamab is a targeted immunotherapy used in the treatment of certain cancers, particularly in pediatric oncology. It represents a significant advancement in addressing challenging forms of disease by leveraging the body’s immune system.
Key Takeaways
- Naxitamab is a monoclonal antibody specifically designed to target the GD2 ganglioside found on neuroblastoma cells.
- Its primary therapeutic use is in treating high-risk neuroblastoma in specific patient populations.
- The drug works by binding to GD2, initiating an immune response that leads to the destruction of cancer cells.
- Common side effects include pain, fever, and infusion-related reactions, with careful management required during administration.
- Dosage is typically administered intravenously, often requiring pre-medication to mitigate potential adverse reactions.
What is Naxitamab?
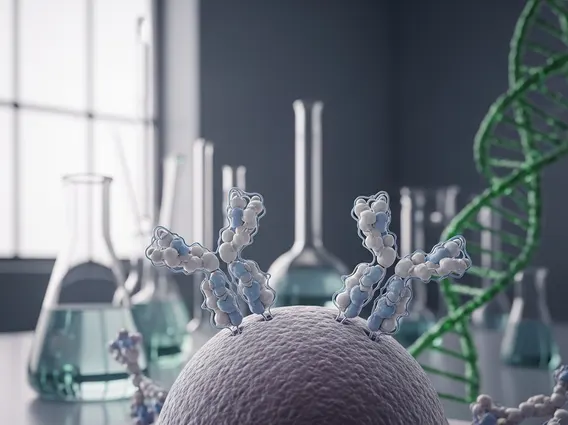
Naxitamab is a humanized monoclonal antibody that serves as a crucial component in the treatment of high-risk neuroblastoma. This innovative therapy specifically targets the GD2 ganglioside, a disialoganglioside that is highly expressed on the surface of neuroblastoma cells but has limited expression on normal tissues. By selectively binding to GD2, naxitamab helps the immune system identify and attack these cancerous cells.
Neuroblastoma is a rare cancer that primarily affects infants and young children, originating from immature nerve cells found in several areas of the body, most commonly in the adrenal glands. Given its aggressive nature and potential for recurrence, effective targeted therapies like naxitamab are vital for improving patient outcomes. The drug’s development focuses on providing a precise therapeutic option for patients who have limited treatment alternatives.
Naxitamab: Mechanism of Action and Therapeutic Uses
The **naxitamab mechanism of action** involves its high-affinity binding to the GD2 ganglioside. Once bound, naxitamab initiates an immune response through several pathways, including antibody-dependent cell-mediated cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC). These processes recruit immune cells and proteins to the tumor site, leading to the destruction of GD2-expressing neuroblastoma cells. This targeted approach minimizes damage to healthy cells, a common challenge with traditional chemotherapy.
Regarding its therapeutic applications, **naxitamab drug information** indicates its use in specific clinical scenarios. It is approved for the treatment of high-risk neuroblastoma in patients who have achieved a partial response, minor response, or stable disease to prior therapy, or who have relapsed or refractory disease. It is typically administered in combination with granulocyte-macrophage colony-stimulating factor (GM-CSF), which further enhances the immune response against cancer cells.
Naxitamab is specifically indicated for:
- Patients with high-risk neuroblastoma in the bone or bone marrow.
- Individuals who have demonstrated a partial response, minor response, or stable disease to prior first-line therapy.
- Patients experiencing relapsed or refractory disease after previous treatments.
This targeted therapy offers a specialized option for children facing a particularly aggressive form of cancer, aiming to improve survival rates and quality of life.
Naxitamab Side Effects and Dosage
Understanding **naxitamab side effects and dosage** is crucial for its safe and effective administration. Like all potent medications, naxitamab can cause a range of adverse reactions. The most common side effects are often related to the infusion process and include severe neuropathic pain, fever, tachycardia, vomiting, diarrhea, and infusion-related reactions such as flushing, rash, and hypotension. Pain management is a significant aspect of treatment, often requiring opioid analgesics and other supportive care measures.
More serious side effects can include hypersensitivity reactions, capillary leak syndrome, and neurological toxicities. Due to the potential for severe reactions, naxitamab is administered in a controlled clinical setting, typically in a hospital. Patients usually receive pre-medication, including antihistamines, antipyretics, and pain relievers, to help mitigate these adverse effects.
The typical dosage of naxitamab is administered intravenously over a period of 30-60 minutes, usually on specific days within a treatment cycle. The exact dose is calculated based on the patient’s body surface area. Treatment cycles are generally repeated every few weeks, with the total number of cycles determined by the patient’s response to therapy and tolerance of side effects. Close monitoring of vital signs and neurological status is essential throughout the infusion and for a period afterward to manage any emerging complications promptly.
