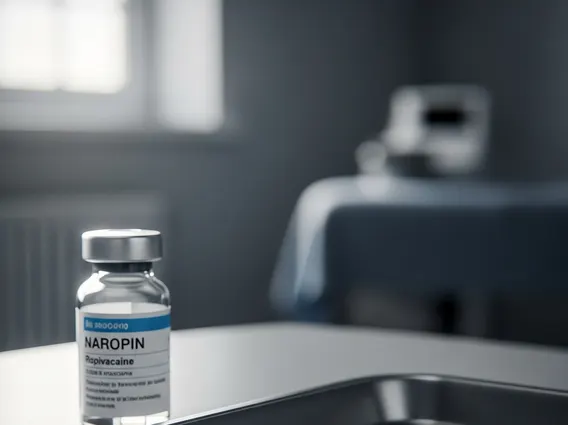
Naropin
Naropin is a widely used local anesthetic, primarily employed to block nerve impulses and provide temporary pain relief or surgical anesthesia. It contains ropivacaine hydrochloride as its active ingredient, making it a crucial medication in various medical procedures.
Key Takeaways
- Naropin is an amide-type local anesthetic containing ropivacaine, used for regional anesthesia and pain management.
- It functions by reversibly blocking sodium channels in nerve membranes, preventing the transmission of pain signals.
- Its primary applications include surgical anesthesia, labor analgesia, and acute pain relief.
- Potential adverse effects range from common reactions like nausea and hypotension to rare but serious systemic toxicity.
- Careful administration, dosage, and patient monitoring are essential to ensure safety and efficacy.
What is Naropin?
Naropin refers to a pharmaceutical preparation whose active ingredient is ropivacaine hydrochloride, an amide-type local anesthetic. It is designed to produce local or regional anesthesia and analgesia by reversibly blocking the initiation and conduction of nerve impulses. This medication is distinct from some other local anesthetics due to its specific pharmacological profile, which includes a favorable safety margin, particularly concerning cardiotoxicity, compared to older agents like bupivacaine. Healthcare professionals administer Naropin to numb specific areas of the body, allowing for pain-free surgical procedures or effective pain management without inducing general unconsciousness.
Naropin Uses and How It Works
Naropin is primarily utilized for both surgical anesthesia and acute pain management, demonstrating its versatility in clinical settings. Its applications span various medical specialties, providing targeted pain relief and facilitating diverse procedures. The mechanism of action for Naropin involves its effects on nerve cells.
Naropin works by stabilizing the neuronal membrane and preventing the influx of sodium ions through voltage-gated sodium channels. This action inhibits the depolarization of the nerve cell membrane, thereby blocking the initiation and conduction of nerve impulses. Consequently, pain signals cannot be transmitted to the brain, leading to a temporary loss of sensation in the affected area. This selective blockade often allows for effective analgesia with minimal impact on motor function, which can be advantageous in certain clinical scenarios.
Common clinical applications for Naropin include:
- Surgical Anesthesia: Used for major nerve blocks (e.g., brachial plexus block), epidural anesthesia for abdominal or lower limb surgery, and field blocks.
- Acute Pain Management: Employed for epidural infusion for post-operative pain, labor analgesia, and continuous peripheral nerve blocks.
- Diagnostic and Therapeutic Blocks: Utilized in pain clinics for various diagnostic and therapeutic nerve blocks to manage chronic pain conditions.
Naropin Side Effects, Warnings, and Drug Information
Comprehensive Naropin drug information is vital for safe and effective use. Like all medications, Naropin can cause side effects, and a thorough understanding of Naropin side effects and warnings is crucial for both patients and healthcare providers. The incidence and severity of side effects are often dose-dependent and can vary based on the site of administration and individual patient factors.
Common side effects associated with Naropin include:
- Nausea and vomiting
- Hypotension (low blood pressure)
- Bradycardia (slow heart rate)
- Headache and dizziness
- Paresthesia (tingling or numbness)
- Urinary retention
More serious, though less common, adverse effects can occur, particularly with accidental intravascular injection or overdose. These may include central nervous system (CNS) toxicity, manifesting as seizures, tremors, or perioral numbness, and cardiovascular toxicity, which can lead to arrhythmias, myocardial depression, and even cardiac arrest. Allergic reactions, though rare, are also possible.
Important warnings include the risk of systemic toxicity, especially in patients with pre-existing cardiac or liver conditions, and the potential for epidural hematoma in patients receiving anticoagulant therapy. Naropin should only be administered by clinicians experienced in regional anesthetic techniques and familiar with the management of potential complications. Dosage must be carefully individualized based on the patient’s physical status, the type of block, and the desired duration of anesthesia or analgesia. Continuous monitoring of vital signs and neurological status is essential during and after administration to detect and manage any adverse reactions promptly.
