Metastasectomy
Metastasectomy is a surgical procedure focused on removing metastatic tumors, which are secondary cancerous growths that have spread from the primary tumor to other parts of the body. This intervention is a critical component of cancer treatment for select patients, aiming to improve outcomes and quality of life.
Key Takeaways
- Metastasectomy involves the surgical removal of metastatic tumors to control cancer spread.
- It is typically considered for patients with oligometastatic disease, where cancer has spread to a limited number of sites.
- The procedure can significantly extend survival and alleviate symptoms for carefully selected individuals.
- Potential benefits include improved prognosis, while risks are similar to those of major surgery.
- Recovery varies based on the extent of surgery and requires comprehensive post-operative care and follow-up.
What is Metastasectomy?
Metastasectomy refers to the surgical excision of tumors that have spread from their original site to distant organs. This procedure is a targeted approach within oncology, primarily employed when cancer has metastasized to a limited number of sites, a condition often termed oligometastatic disease. The goal of metastasectomy can range from achieving a cure in highly selected cases to extending life expectancy, alleviating symptoms, or improving the effectiveness of other cancer treatments.
While cancer metastasis generally indicates advanced disease, advancements in surgical techniques and systemic therapies have made metastasectomy a viable option for a growing number of patients. The decision to perform a metastasectomy is made by a multidisciplinary team of specialists, considering factors such as the primary cancer type, the number and location of metastases, the patient’s overall health, and the potential for complete tumor removal. According to the National Cancer Institute, for certain cancers like colorectal cancer with liver metastases, surgical removal of metastases can lead to significantly improved long-term survival rates in carefully selected patients.
Metastasectomy Procedure Details, Benefits, and Risks
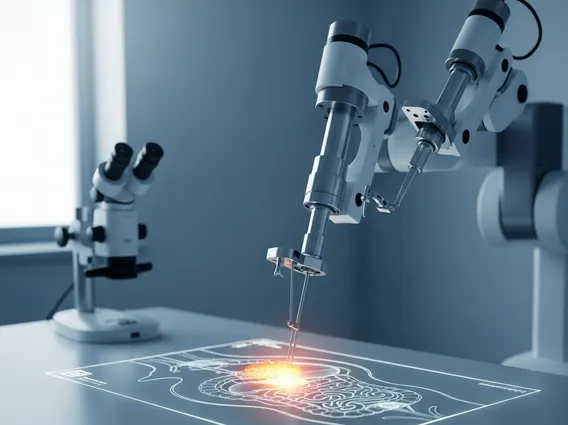
The execution of a metastasectomy is highly individualized, depending on the location and characteristics of the metastatic tumors. Metastasectomy procedure details involve extensive pre-operative planning, including advanced imaging techniques such as CT scans, MRI, and PET scans, to precisely map the tumors. Surgical approaches can vary widely, from traditional open surgery to minimally invasive techniques like laparoscopy, thoracoscopy, or robotic-assisted surgery, which often result in smaller incisions, reduced pain, and faster recovery times. Common sites for metastasectomy include the lungs, liver, brain, and bones, reflecting the most frequent locations for cancer spread. The surgery is often performed in conjunction with other treatments, such as chemotherapy, radiation therapy, or targeted therapies, to maximize therapeutic outcomes.
The benefits of metastasectomy can be substantial for appropriate candidates. For many, it offers the best chance for long-term survival or even cure, particularly in cases of oligometastatic disease where all visible tumors can be removed. Beyond survival, the procedure can significantly improve a patient’s quality of life by relieving symptoms caused by the tumors, such as pain, obstruction, or organ dysfunction. For instance, removing a tumor compressing a nerve can alleviate severe pain. Studies have shown that for specific cancers, such as those originating in the colon or rectum and spreading to the liver, metastasectomy can achieve 5-year survival rates of 25-50% in selected patient populations.
However, like any major surgical intervention, there are inherent risks of metastasectomy. These include general surgical complications such as bleeding, infection, adverse reactions to anesthesia, and blood clots. Specific risks are also associated with the organ being operated on; for example, lung metastasectomy carries risks of pneumothorax (collapsed lung) or prolonged air leak, while liver metastasectomy can lead to liver dysfunction or bile leakage. There is also the risk of incomplete tumor removal or recurrence of the cancer, necessitating ongoing surveillance and potentially further treatment. A thorough discussion with the surgical team about potential benefits versus risks is crucial for informed decision-making.
Metastasectomy Recovery Process
The Metastasectomy recovery process is a critical phase that varies significantly based on the extent of the surgery, the organs involved, and the patient’s overall health. Immediately following the procedure, patients typically remain in the hospital for several days to weeks for close monitoring, pain management, and initial rehabilitation. Pain control is a priority, often managed with a combination of medications to ensure comfort and facilitate early mobilization. Depending on the surgical site, patients may have drains, catheters, or other medical devices that are gradually removed as recovery progresses.
Short-term recovery involves a gradual return to daily activities. Patients are often encouraged to engage in light physical activity, such as walking, to prevent complications like blood clots and to rebuild strength. Dietary adjustments may be necessary, especially after abdominal surgeries. Fatigue is a common and often prolonged side effect of cancer treatment and surgery, requiring patience and adequate rest. Physical therapy and rehabilitation programs are frequently recommended to help restore function and mobility, particularly after extensive procedures or those affecting limbs.
Long-term recovery involves ongoing medical follow-up, which is essential for monitoring for any signs of cancer recurrence. This typically includes regular imaging scans (CT, MRI, PET) and blood tests. Many patients will continue with other forms of oncological treatment, such as chemotherapy, radiation, or targeted therapy, as part of their comprehensive cancer management plan. Psychological support, including counseling or support groups, can also be invaluable in navigating the emotional challenges associated with cancer recovery and surveillance. A full return to normal activities can take several months, and patients are advised to follow their healthcare team’s guidance closely to ensure the best possible outcome.