Merkel Cell
Merkel Cell Carcinoma is a rare and aggressive form of skin cancer that originates from Merkel cells, which are found in the top layer of the skin. This article provides a comprehensive overview of this condition, covering its characteristics, contributing factors, and available treatment approaches.
Key Takeaways
- Merkel Cell Carcinoma (MCC) is a rare and aggressive skin cancer, primarily affecting sun-exposed areas.
- It often presents as a fast-growing, painless, firm nodule, commonly on the head, neck, or limbs.
- The Merkel cell polyomavirus (MCPyV) is a significant contributing factor in most cases, alongside UV radiation exposure and immunosuppression.
- Early detection is crucial for effective treatment, which typically involves surgery, radiation, and increasingly, immunotherapy.
- Due to its aggressive nature and high recurrence rate, a multidisciplinary approach to management is essential.
What is Merkel Cell Carcinoma?
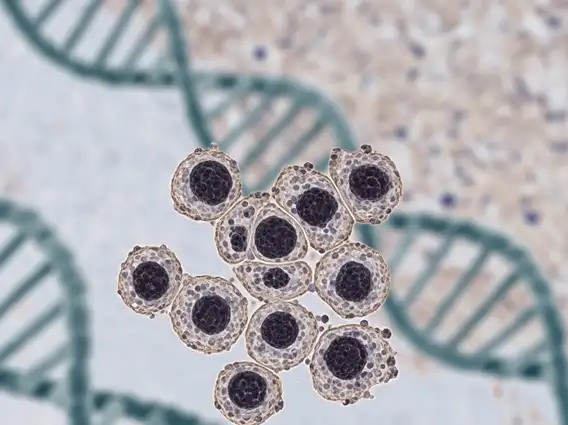
Merkel Cell Carcinoma (MCC) is a rare and highly aggressive type of skin cancer that develops from Merkel cells, which are specialized neuroendocrine cells located in the epidermis (the outermost layer of the skin). These cells are thought to play a role in touch sensation. MCC is characterized by its rapid growth and high potential for metastasis, meaning it can spread quickly to nearby lymph nodes and distant organs. While relatively uncommon, its incidence has been increasing, particularly among older adults.
Understanding what is Merkel Cell Carcinoma involves recognizing its distinct cellular origin and aggressive behavior. It is distinct from other common skin cancers like melanoma or basal cell carcinoma due to its specific cell type and often viral association. The disease typically affects sun-exposed areas of the body, such as the head, neck, and extremities, but can occur anywhere on the skin.
Merkel Cell Carcinoma: Signs, Causes, and Risk Factors
Recognizing merkel cell cancer symptoms and signs early is vital for improving prognosis. MCC often appears as a single, firm, painless, shiny, or dome-shaped nodule (lump) on the skin. These lesions tend to grow rapidly and may be red, pink, or purple. They are most commonly found on areas of the body frequently exposed to the sun, such as the face, neck, and arms. Due to its painless nature, it can sometimes be overlooked or mistaken for a benign cyst or insect bite, leading to delays in diagnosis.
Understanding merkel cell carcinoma causes and risk factors is crucial for prevention and early detection. The primary cause is strongly linked to the Merkel cell polyomavirus (MCPyV), which is found in about 80% of MCC tumors. While many people are exposed to MCPyV, only a small fraction develop MCC, suggesting other factors are at play. Key risk factors include:
- Ultraviolet (UV) Radiation Exposure: Prolonged exposure to sunlight or artificial UV light (e.g., tanning beds) significantly increases risk.
- Immunosuppression: Individuals with weakened immune systems, such as organ transplant recipients, those with HIV/AIDS, or people undergoing chemotherapy, have a substantially higher risk.
- Fair Skin: People with fair skin, light hair, and light eyes are more susceptible to sun damage and, consequently, MCC.
- Age: The risk of MCC increases with age, with most diagnoses occurring in individuals over 50.
These factors often work in combination, contributing to the development and progression of this aggressive cancer.
Merkel Cell Carcinoma Treatment Options
Effective merkel cell carcinoma treatment options typically involve a multidisciplinary approach due to the cancer’s aggressive nature and high potential for recurrence and metastasis. The choice of treatment depends on the stage of the cancer, its location, the patient’s overall health, and whether it has spread to lymph nodes or other parts of the body. The primary modalities include:
Surgery: Surgical removal of the primary tumor is often the first step. This may involve wide local excision to ensure clear margins, sometimes followed by sentinel lymph node biopsy to check for spread to nearby lymph nodes. If lymph nodes are involved, a complete lymph node dissection may be performed.
Radiation Therapy: Radiation is frequently used after surgery to destroy any remaining cancer cells in the tumor bed or regional lymph nodes, reducing the risk of local recurrence. It can also be used as a primary treatment for tumors that cannot be surgically removed or for metastatic disease to alleviate symptoms.
Systemic Therapies: For advanced or metastatic MCC, systemic treatments are crucial. These include:
- Chemotherapy: While historically used, chemotherapy often provides temporary responses and can have significant side effects.
- Immunotherapy: This has revolutionized MCC treatment. Immune checkpoint inhibitors, such as pembrolizumab and avelumab, work by boosting the body’s immune response against cancer cells. These drugs have shown durable responses in many patients with advanced MCC and are now a preferred treatment for metastatic disease.
Clinical trials are continuously exploring new and more effective treatments, including targeted therapies. The aggressive nature of MCC necessitates close follow-up and surveillance after treatment to monitor for recurrence.
