Intravasation
Intravasation is a critical biological process where cells penetrate the walls of blood or lymphatic vessels to enter the circulatory system. This phenomenon is particularly significant in the context of cancer, as it represents a pivotal step in the metastatic cascade, enabling cancer cells to disseminate from a primary tumor to distant sites within the body.
Key Takeaways
- Intravasation is the process of cells entering blood or lymphatic vessels.
- It is a crucial step in cancer metastasis, allowing tumor cells to spread.
- The process involves complex interactions between cancer cells and the tumor microenvironment.
- Cellular changes, such as increased motility and enzymatic activity, facilitate vessel penetration.
- Understanding intravasation is vital for developing strategies to prevent cancer dissemination.
What is Intravasation?
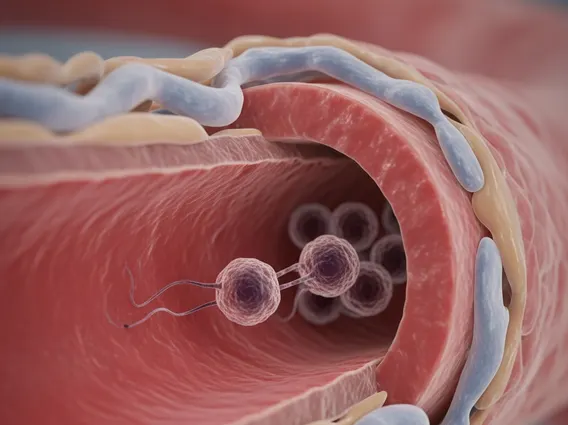
Intravasation refers to the complex biological process by which cells, predominantly cancer cells, breach the basement membrane and endothelial lining of a blood or lymphatic vessel to gain access to the circulatory system. This is a fundamental event in the spread of cancer, as it allows malignant cells to leave the primary tumor site and travel through the body. The Intravasation meaning and process involves a series of coordinated steps, requiring changes in cell behavior and interaction with the surrounding microenvironment. It is distinct from extravasation, which is the subsequent process of cells exiting the vasculature at a distant site to form secondary tumors.
For cancer cells, successful intravasation is a prerequisite for systemic dissemination and the formation of metastases. Without the ability to enter the bloodstream or lymphatic system, tumor cells would remain confined to their original location. This process highlights the adaptability and invasive potential of cancer cells, which can remodel their immediate surroundings and overcome physical barriers to achieve systemic spread.
The Process of Intravasation
The mechanism of intravasation is intricate, involving several stages and interactions between cancer cells, stromal cells, and the vascular endothelium. It typically begins with cancer cells detaching from the primary tumor mass and migrating through the extracellular matrix (ECM) towards nearby blood or lymphatic vessels. This migration is often facilitated by proteolytic enzymes, such as matrix metalloproteinases (MMPs), secreted by both tumor cells and associated stromal cells, which degrade the ECM and create pathways for invasion.
Once at the vessel wall, cancer cells interact with the endothelial cells lining the vessel. This interaction can involve adhesion molecules and signaling pathways that promote the retraction of endothelial cells or direct penetration through the endothelial cell layer. The process can be summarized by several key steps:
- Detachment and Migration: Cancer cells detach from the primary tumor and migrate through the interstitial stroma.
- ECM Degradation: Enzymes break down the extracellular matrix, clearing a path to the vessel.
- Vessel Interaction: Tumor cells adhere to the outer surface of the blood or lymphatic vessel.
- Endothelial Barrier Breach: Cells penetrate the endothelial cell layer, either by squeezing between cells or directly through them.
- Entry into Lumen: The cancer cells successfully enter the vessel lumen, gaining access to the circulation.
The tumor microenvironment plays a crucial role, with factors like inflammation, hypoxia, and growth factors influencing the efficiency of intravasation. Macrophages, for instance, can form “tumor microenvironment of metastasis” (TMEM) doorways, facilitating the entry of tumor cells into vessels.
Intravasation in Cancer Metastasis
The significance of Intravasation in cancer metastasis cannot be overstated, as it is the gateway for cancer cells to spread throughout the body. Once cancer cells successfully intravasate, they become circulating tumor cells (CTCs). These CTCs travel through the bloodstream or lymphatic system, potentially reaching distant organs. However, the journey through the circulation is perilous; many CTCs succumb to shear stress, immune attack, or anoikis (a form of programmed cell death induced by loss of cell-matrix attachment).
Despite these challenges, a subset of CTCs survives and eventually extravasates, exiting the vessel at a secondary site to form new metastatic tumors. Metastasis is responsible for approximately 90% of cancer-related deaths, underscoring the critical role of processes like intravasation in disease progression. (Source: National Cancer Institute). Understanding the molecular mechanisms governing intravasation offers promising avenues for therapeutic intervention. By targeting the factors and pathways that enable cancer cells to enter the vasculature, researchers aim to develop strategies to inhibit or prevent the spread of cancer, thereby improving patient outcomes and reducing the burden of metastatic disease.