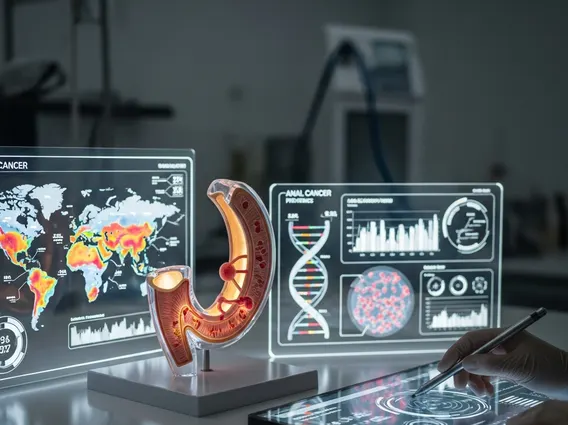
Global Statistics on Anal Cancer
Anal cancer, though relatively rare compared to other malignancies, presents a growing public health concern worldwide. Understanding its global statistical landscape is crucial for effective prevention strategies, early detection, and improved patient outcomes.
Key Takeaways
- The incidence of anal cancer globally has been steadily rising over the past few decades, impacting both men and women.
- Human Papillomavirus (HPV) infection is the primary causal agent, accounting for a significant majority of cases worldwide.
- Significant regional variations exist in anal cancer prevalence worldwide, influenced by factors like HPV vaccination rates, HIV prevalence, and lifestyle.
- Early detection and advancements in treatment have led to improved survival rates, though anal cancer mortality rates international still highlight disparities.
- Public health initiatives focusing on HPV vaccination and awareness are vital in mitigating the future burden of this disease.
Global Anal Cancer Statistics Overview
A comprehensive look at global anal cancer statistics reveals important trends and disparities across different populations. While it remains less common than many other cancers, its incidence has shown a concerning upward trajectory in recent decades. This increase underscores the need for enhanced surveillance and targeted interventions to address the rising burden of the disease.
Worldwide Incidence and Prevalence
The incidence of anal cancer globally refers to the rate of new cases diagnosed each year, while anal cancer prevalence worldwide indicates the total number of people living with the condition at a given time. According to GLOBOCAN 2020 estimates from the International Agency for Research on Cancer (IARC), there were approximately 51,000 new cases of anal cancer diagnosed globally, resulting in about 19,000 deaths. The age-standardized incidence rate was around 0.6 per 100,000 population. These figures highlight that while it is not among the most common cancers, its impact is significant, particularly given the rising trends. The prevalence reflects a growing number of individuals who have been diagnosed, many of whom are living longer due to improved treatments.
Regional Variations and Hotspots
Analysis of worldwide data on anal cancer cases reveals considerable regional variations. North America, Western Europe, and Australia/New Zealand tend to report higher incidence rates compared to many parts of Asia and Africa. For instance, countries like the United States and the Netherlands show some of the highest rates globally. These disparities are often attributed to a complex interplay of factors including differences in the prevalence of Human Papillomavirus (HPV) infection, HIV prevalence, access to healthcare and screening, and lifestyle factors such as smoking. Regions with higher rates of HIV infection, particularly among men who have sex with men (MSM), often experience a disproportionately higher burden of anal cancer due to the synergistic effect of HIV and HPV on cancer development.
Mortality and Survival Rates Globally
Understanding anal cancer mortality rates international and survival statistics is critical for assessing the effectiveness of treatment strategies and identifying areas for improvement in global health initiatives. While the incidence of anal cancer has been rising, advancements in medical science and earlier detection have contributed to more favorable outcomes for many patients.
International Trends in Fatalities
Despite the increase in incidence, anal cancer mortality rates international have shown some stabilization or even slight decline in certain high-income countries, largely due to improved diagnostic techniques and more effective treatment modalities. However, disparities persist, with lower-income regions often facing higher mortality rates due to limited access to advanced medical care, late-stage diagnoses, and inadequate treatment infrastructure. The overall trend indicates that while more people are being diagnosed, a greater proportion are surviving, particularly in settings with robust healthcare systems. This suggests that the global burden of anal cancer is shifting from high mortality to a focus on long-term survivorship and quality of life.
Factors Influencing Prognosis
Several factors significantly influence the prognosis and survival rates for individuals diagnosed with anal cancer. The most critical factor is the stage of cancer at diagnosis; localized disease has a much better prognosis than regional or distant metastatic disease. Early detection through awareness and screening programs is therefore paramount. Other influential factors include the patient’s overall health status, immune system strength (e.g., HIV-positive individuals may have a poorer prognosis if not adequately managed), and access to multidisciplinary care teams. Treatment adherence, including chemotherapy and radiation therapy, also plays a crucial role in determining long-term survival. Advances in treatment protocols, such as intensity-modulated radiation therapy (IMRT) and concurrent chemoradiation, have significantly improved local control and reduced treatment-related toxicities, contributing to better outcomes.
Key Risk Factors and Epidemiological Insights
The epidemiology of anal cancer global is largely driven by a clear set of risk factors, with Human Papillomavirus (HPV) being the most prominent. Understanding these factors is essential for developing effective prevention strategies and public health campaigns.
HPV and Other Causal Agents
Human Papillomavirus (HPV), particularly high-risk types like HPV-16 and HPV-18, is the primary etiological agent for anal cancer, responsible for approximately 85-90% of all cases. HPV infection is sexually transmitted and can lead to precancerous lesions (anal intraepithelial neoplasia, AIN) that may progress to invasive cancer over time. Other significant risk factors include:
- HIV Infection: Individuals living with HIV are at a substantially increased risk, as their compromised immune systems are less able to clear HPV infections, leading to persistent infection and progression to cancer.
- Immunosuppression: Organ transplant recipients and others on immunosuppressive medications also face elevated risks.
- Smoking: Tobacco smoking is an independent risk factor that further increases the likelihood of developing anal cancer, potentially by impairing immune function and promoting HPV persistence.
- History of other HPV-related cancers: A history of cervical, vulvar, vaginal, or penile cancer increases the risk of anal cancer.
- Chronic inflammation: Conditions leading to chronic inflammation in the anal region might also contribute, though this is less definitively established than HPV and HIV.
Demographic Patterns (Age, Sex, Geography)
Anal cancer statistics show distinct demographic patterns. The disease is more common in older adults, with the median age at diagnosis typically in the sixth or seventh decade of life, although it can occur at any age. Historically, anal cancer was more prevalent in women, but recent trends indicate a rising incidence among men, particularly among men who have sex with men (MSM), largely due to higher rates of HPV and HIV co-infection in this population. Geographically, as mentioned, incidence rates vary significantly, reflecting differences in risk factor prevalence and healthcare infrastructure. These demographic insights are crucial for targeting screening and vaccination efforts to the most vulnerable populations, thereby improving the overall epidemiology of anal cancer global.
Trends in Anal Cancer Diagnoses
The landscape of anal cancer statistics is dynamic, with notable shifts in diagnosis patterns over time. Understanding these trends is vital for public health planning and resource allocation, especially as the global health community grapples with the rising incidence of this disease.
Changes Over Time and Projections
Over the past few decades, there has been a consistent increase in the diagnosis of anal cancer globally. This upward trend is observed in many countries, particularly in high-income regions. For instance, data from the United States and several European countries indicate a steady rise in incidence rates for both men and women. This increase is partly attributable to improved diagnostic techniques and greater awareness, but primarily reflects the increasing prevalence of key risk factors, especially persistent HPV infection and the aging population. Projections suggest that this upward trend is likely to continue in the coming years, underscoring the urgency of implementing effective prevention and early detection strategies to mitigate the future burden of the disease. These projections are critical for healthcare systems to anticipate future needs in oncology services.
Impact of Screening and Awareness
The impact of screening and awareness campaigns on anal cancer statistics is significant. While routine population-wide screening for anal cancer is not universally recommended, targeted screening for high-risk groups, such as HIV-positive individuals and MSM, using anal Pap tests and high-resolution anoscopy, has shown promise in detecting precancerous lesions (AIN) that can be treated before progressing to invasive cancer. Increased public awareness about HPV, its link to anal cancer, and the availability of HPV vaccines are crucial. HPV vaccination programs, particularly when administered before exposure to the virus, are highly effective in preventing HPV-related cancers, including anal cancer. As vaccination rates increase globally, a long-term decline in HPV-associated anal cancer incidence is anticipated, though the full impact will take decades to materialize due to the long latency period of the disease.
Frequently Asked Questions
What are the primary risk factors for anal cancer?
The most significant risk factor for anal cancer is infection with high-risk types of Human Papillomavirus (HPV), particularly HPV-16 and HPV-18. Other major risk factors include being infected with Human Immunodeficiency Virus (HIV), which compromises the immune system’s ability to clear HPV. Additionally, a history of smoking, immunosuppression due to organ transplantation, and a history of other HPV-related cancers (such as cervical or vulvar cancer) significantly increase an individual’s risk of developing anal cancer.
Is anal cancer incidence increasing globally?
Yes, the incidence of anal cancer globally has been steadily increasing over the past few decades in many parts of the world, particularly in high-income countries. This rise is attributed to several factors, including the persistent prevalence of high-risk HPV infections, the aging global population, and improved diagnostic capabilities. The increase is notable in both men and women, with a particularly pronounced rise among specific high-risk groups, such as men who have sex with men and individuals living with HIV.
How does early detection impact anal cancer prognosis?
Early detection significantly improves the prognosis and survival rates for individuals with anal cancer. When anal cancer is diagnosed at a localized stage, before it has spread to regional lymph nodes or distant sites, the five-year survival rate is substantially higher. Early detection allows for more effective and less invasive treatment options, often leading to better outcomes and reduced treatment-related morbidity. Awareness of symptoms and targeted screening for high-risk populations are crucial for achieving earlier diagnoses and improving overall patient survival.
