Endoscopic Retrograde Cholangiopancreatography
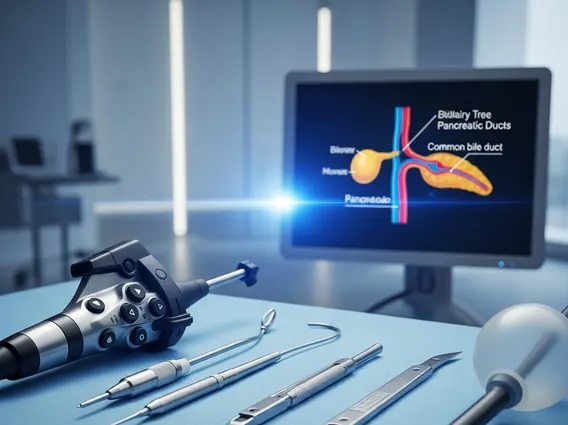
Endoscopic Retrograde Cholangiopancreatography is a specialized medical procedure used to diagnose and treat conditions affecting the bile ducts, pancreatic duct, and gallbladder. This technique combines endoscopy and fluoroscopy to visualize and intervene in these critical digestive pathways.
Key Takeaways
- Endoscopic Retrograde Cholangiopancreatography (ERCP) is a procedure combining endoscopy and X-ray imaging to examine and treat issues in the bile and pancreatic ducts.
- It is primarily used for diagnosing conditions like gallstones, strictures, and tumors, and for therapeutic interventions such as stone removal or stent placement.
- The procedure involves inserting an endoscope through the mouth, stomach, and duodenum to access the ducts.
- Common risks include pancreatitis, infection, bleeding, and perforation, though serious complications are rare.
- Recovery typically involves a short hospital stay for monitoring, with most patients resuming normal activities within a few days.
What is Endoscopic Retrograde Cholangiopancreatography (ERCP)?
Endoscopic Retrograde Cholangiopancreatography (ERCP) is a sophisticated medical procedure that allows physicians to diagnose and treat problems in the liver, gallbladder, bile ducts, and pancreas. This technique combines the use of an endoscope—a thin, flexible, lighted tube with a camera—and X-ray imaging (fluoroscopy). The endoscope is guided through the mouth, esophagus, stomach, and into the duodenum, where the bile and pancreatic ducts open.
The process of Endoscopic Retrograde Cholangiopancreatography explained involves the insertion of a catheter into the bile or pancreatic ducts through the endoscope. A contrast dye is then injected, which allows these ducts to become visible on X-ray images. This visualization helps identify abnormalities such as gallstones, strictures (narrowing), blockages, or tumors. ERCP is unique in its ability to offer both diagnostic clarity and immediate therapeutic intervention during the same session.
ERCP Procedure for Diagnosis and Treatment
The ERCP procedure for diagnosis and treatment is typically performed in a hospital or outpatient surgical center. Patients are usually given sedation to ensure comfort throughout the procedure, which can last from 30 minutes to several hours depending on the complexity. Once the endoscope reaches the opening of the bile and pancreatic ducts (the ampulla of Vater), a small catheter is passed through the endoscope and into the desired duct.
Diagnostic applications include identifying the cause of unexplained abdominal pain, jaundice, or abnormal liver function tests. Therapeutically, ERCP is highly effective for a range of conditions. For instance, it can be used to remove gallstones or other blockages from the bile duct, widen narrowed ducts using balloons, or insert stents to keep ducts open. It can also be used to take tissue samples (biopsies) for further analysis, which is crucial for diagnosing cancers of the bile duct or pancreas. The ability to perform both diagnostic and therapeutic maneuvers in one sitting often reduces the need for multiple procedures.
Risks and Recovery from ERCP Procedure
While generally safe, there are potential Risks and recovery from ERCP procedure that patients should be aware of. The most common and significant complication is pancreatitis, an inflammation of the pancreas, which occurs in about 3-5% of cases. Other potential risks include infection of the bile ducts (cholangitis), bleeding, and, rarely, perforation of the duodenum or bile duct. These complications often require hospitalization and further medical intervention.
Following an ERCP, patients are monitored closely in a recovery area until the effects of sedation wear off. Most individuals experience some throat soreness, bloating, or mild abdominal discomfort. Patients are typically advised to avoid eating or drinking for a few hours post-procedure and to gradually reintroduce fluids and light foods. Depending on the complexity of the procedure and the patient’s overall health, a short hospital stay for observation may be recommended, especially if therapeutic interventions were performed. Full recovery usually occurs within a few days, with patients able to resume their normal activities.
