Embolization
Embolization is a minimally invasive medical procedure designed to block blood flow to specific areas of the body. This technique is utilized to treat a variety of conditions, ranging from stopping active bleeding to shrinking tumors or addressing vascular malformations.
Key Takeaways
- Embolization is a minimally invasive procedure that intentionally blocks blood vessels.
- It is used to treat conditions such as tumors, aneurysms, and active bleeding.
- The procedure involves guiding a catheter to the target vessel and releasing embolic agents.
- Various types of embolization exist, tailored to the specific medical condition.
- Recovery typically involves managing pain and restricting activity, with potential for minor side effects.
What is Embolization?
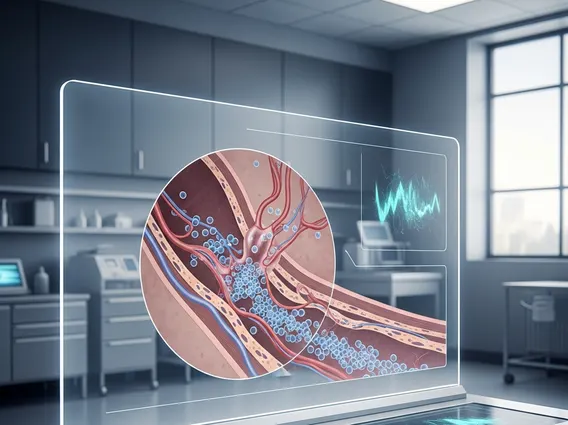
Embolization refers to a sophisticated medical procedure performed by interventional radiologists to intentionally block or reduce blood flow in a blood vessel. This technique is employed for therapeutic purposes, such as stopping hemorrhage, depriving tumors of their blood supply, or correcting vascular abnormalities like aneurysms or arteriovenous malformations (AVMs). The principle behind embolization involves introducing various embolic agents into the target vessel, which then occlude it, preventing blood from reaching the intended area.
The procedure is typically performed under image guidance, allowing the specialist to navigate precisely through the body’s vascular network. By cutting off the blood supply, embolization can effectively shrink abnormal growths, halt internal bleeding, or prevent rupture of weakened blood vessels, offering a less invasive alternative to traditional open surgery in many cases.
Embolization Procedure: Types and Applications
The embolization procedure involves several key steps. Initially, a small incision is made, usually in the groin or wrist, to access an artery. A thin, flexible tube called a catheter is then inserted and guided through the blood vessels to the specific area requiring treatment, using real-time imaging like fluoroscopy. Once positioned, tiny particles, coils, glue, or other embolic agents are released through the catheter to block the blood vessel. The choice of embolic agent depends on the specific condition being treated and the size of the vessel.
The effectiveness of embolization treatment explained through its wide range of applications. For instance, it is commonly used to treat uterine fibroids, where it is known as uterine fibroid embolization (UFE). According to the Society of Interventional Radiology (SIR), UFE is effective in 85-90% of women, providing significant improvement in symptoms. Other applications include treating liver tumors, kidney tumors, gastrointestinal bleeding, brain aneurysms, and varicoceles. There are several types of embolization therapy, each suited for different clinical scenarios:
- Particle Embolization: Uses small beads or particles to block tiny blood vessels, often used for tumors or fibroids.
- Coil Embolization: Involves placing platinum coils into a vessel to promote clotting and occlusion, common for aneurysms or bleeding.
- Liquid Embolization: Utilizes a liquid embolic agent that solidifies upon contact with blood, creating a cast within the vessel, frequently used for AVMs.
- Gel Foam Embolization: Employs absorbable gelatin sponge particles for temporary occlusion, often used to control acute bleeding.
These diverse techniques allow interventional radiologists to tailor the approach to each patient’s unique needs, maximizing efficacy while minimizing risks.
Embolization Side Effects and Recovery
Patients undergoing embolization may experience various embolization side effects recovery challenges. Common side effects include pain at the embolization site, nausea, vomiting, and a low-grade fever, often referred to as post-embolization syndrome. These symptoms are usually temporary and can be managed with medication. Less common but more serious complications can include infection, damage to surrounding tissues, or non-target embolization, where embolic agents inadvertently block healthy blood vessels. The risk of such complications is generally low due to the precision of image-guided techniques.
Recovery time varies depending on the specific procedure and the patient’s overall health. Most patients require a hospital stay of one to three days for observation and pain management. During the initial recovery period, it is common to feel fatigued and experience discomfort. Patients are typically advised to avoid strenuous activities for a few weeks and to follow up with their doctor for monitoring. Full recovery can take several weeks to a few months, during which the body adapts to the altered blood flow. Adherence to post-procedure instructions and regular follow-up appointments are crucial for a successful outcome and to address any lingering concerns.
