Coloanal Anastomosis
Coloanal anastomosis is a critical surgical procedure often performed following the removal of a diseased or cancerous rectum. This operation aims to restore bowel continuity and function, significantly impacting a patient’s quality of life.
Key Takeaways
- Coloanal anastomosis is a surgical procedure that reconnects the colon to the anus after rectal removal.
- It is primarily performed to treat rectal cancer, inflammatory bowel disease, or other severe rectal conditions.
- The procedure involves carefully joining the healthy colon to the anal canal, often requiring a temporary stoma.
- Recovery typically spans several weeks to months, focusing on bowel function restoration and stoma reversal.
- Potential complications include anastomotic leak, stricture, and changes in bowel habits.
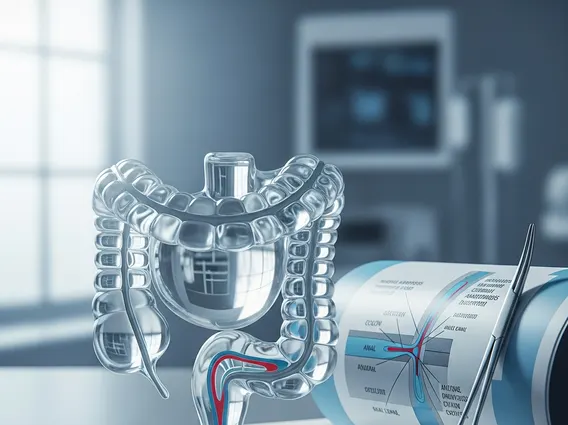
What is Coloanal Anastomosis?
Coloanal anastomosis refers to a surgical technique where the colon (large intestine) is directly connected to the anal canal after the surgical removal of the rectum. This procedure is a vital component of restorative proctocolectomy or low anterior resection, primarily indicated for patients undergoing surgery for rectal cancer, severe inflammatory bowel disease (such as ulcerative colitis), or other conditions necessitating rectal excision. The goal is to preserve natural defecation by re-establishing the continuity of the digestive tract, thereby avoiding a permanent colostomy in many cases.
The success of coloanal anastomosis depends on several factors, including the patient’s overall health, the extent of the disease, and the surgeon’s expertise. It represents a significant advancement in colorectal surgery, allowing many patients to maintain a good quality of life post-surgery, despite the extensive nature of the intervention. According to the American Cancer Society, rectal cancer is a significant concern, and surgical options like this are crucial for treatment and recovery.
The Coloanal Anastomosis Procedure
The Coloanal anastomosis procedure typically involves several key steps, performed under general anesthesia. Initially, the diseased portion of the rectum is carefully resected. The extent of this resection depends on the pathology, such as the size and location of a tumor. Following the removal, the remaining healthy colon is mobilized and brought down to the anal canal. The anastomosis, or surgical connection, is then created between the colon and the anal canal. This connection can be made by hand-sewing or using specialized stapling devices.
In many cases, a temporary diverting stoma (ileostomy or colostomy) is created in the abdominal wall during the initial surgery. This stoma diverts fecal matter away from the newly formed anastomosis, allowing it to heal without contamination. The stoma is usually reversed in a subsequent surgery once the anastomosis has fully healed, typically after 8-12 weeks. The decision to create a temporary stoma is based on factors like the height of the anastomosis, the patient’s health, and the presence of any risk factors for anastomotic leakage.
Coloanal Anastomosis Recovery and Potential Complications
The Coloanal anastomosis recovery time varies significantly among individuals but generally involves a hospital stay of several days to a week, followed by a longer period of recuperation at home. During the initial recovery phase, pain management, fluid balance, and monitoring for early complications are paramount. Patients gradually resume oral intake and begin to mobilize. Once discharged, patients must adapt to living with a temporary stoma, if one was created, and manage their diet to minimize bowel irritation.
Potential Coloanal anastomosis complications can range from minor issues to severe, life-threatening events. Awareness of these risks is crucial for both patients and healthcare providers. Common complications include:
- Anastomotic Leak: This is a serious complication where the surgical connection fails to heal properly, leading to leakage of bowel contents into the abdominal cavity. It can cause infection and sepsis.
- Anastomotic Stricture: Narrowing of the anastomosis can occur due to scar tissue formation, leading to difficulty with bowel movements. This may require endoscopic dilation or further surgery.
- Bowel Dysfunction: Patients may experience changes in bowel habits, such as increased frequency, urgency, or incontinence, due to the removal of the rectum’s reservoir function.
- Infection: Surgical site infections or intra-abdominal infections can occur, requiring antibiotic treatment or drainage.
- Bleeding: Post-operative bleeding at the surgical site is a potential risk.
Long-term recovery focuses on optimizing bowel function and managing any persistent symptoms. Patients often benefit from dietary modifications, pelvic floor exercises, and, in some cases, medication to regulate bowel movements. Regular follow-up with the surgical team and gastroenterologist is essential to monitor recovery and address any emerging issues.
