Causes of Bowel Obstruction in Cancer Patients
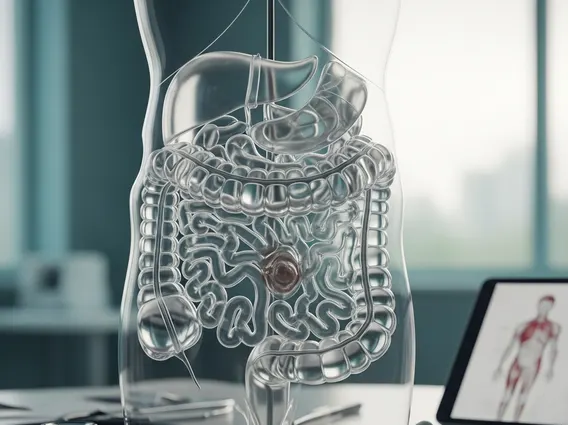
Bowel obstruction is a serious and potentially life-threatening complication that can arise in individuals battling cancer. Understanding the causes of bowel obstruction in cancer patients is crucial for timely diagnosis and effective management, as it significantly impacts quality of life and treatment outcomes.
Key Takeaways
- Direct tumor growth, both primary and metastatic, is a leading cause of physical blockage in the bowel.
- Cancer treatments like radiation and surgery can induce scar tissue or adhesions, leading to obstruction.
- Chemotherapy and opioid medications often impair bowel motility, causing functional obstructions.
- Pre-existing abdominal adhesions and electrolyte imbalances are additional risk factors for bowel obstruction cancer patients face.
- A comprehensive understanding of these factors is vital for managing and preventing this challenging complication.
Direct Tumor-Related Causes of Bowel Obstruction
One of the most direct and concerning causes of bowel obstruction in cancer patients stems from the physical presence and growth of the tumor itself. This can manifest in several ways, directly impeding the passage of food and waste through the digestive tract. The etiology of bowel obstruction in oncology often points to the mechanical blockage caused by malignant tissue.
Primary Tumor Growth & Compression
A primary tumor, originating within or near the gastrointestinal tract, can grow to a size that physically obstructs the bowel lumen. Cancers of the colon, rectum, stomach, and pancreas are particularly prone to causing such blockages. As the tumor expands, it narrows the passageway, making it difficult for contents to move through. This compression can lead to a partial or complete blockage, resulting in symptoms like abdominal pain, distension, nausea, and vomiting. For instance, a large colorectal tumor can directly occlude the colon, preventing stool passage. Reliable statistics indicate that approximately 15-20% of patients with advanced colorectal cancer will develop a bowel obstruction at some point during their disease course, highlighting this significant risk factor. (Source: National Cancer Institute)
Metastatic Disease to the Bowel
Beyond primary tumor growth, metastatic disease is another significant reason why cancer patients get bowel obstruction. Cancer cells can spread from their original site to other parts of the body, including the bowel. The peritoneum, the membrane lining the abdominal cavity and covering the abdominal organs, is a common site for metastatic spread, especially from ovarian, gastric, pancreatic, and colorectal cancers. When cancer cells implant and grow on the bowel surface or within the bowel wall, they can cause extrinsic compression, intrinsic narrowing, or even diffuse infiltration, leading to a cancer related intestinal obstruction causes. These metastatic lesions can create multiple points of obstruction, making management particularly challenging. The presence of peritoneal carcinomatosis, for example, is a frequent cause of malignant bowel obstruction, accounting for a substantial portion of cases in advanced cancer.
Treatment-Induced Bowel Obstruction in Cancer Patients
While cancer treatments are designed to save lives, they can sometimes lead to complications, including bowel obstruction. Understanding these iatrogenic bowel blockage reasons cancer patients experience is crucial for comprehensive care planning and symptom management. These obstructions are often a result of the body’s response to therapeutic interventions.
Radiation Therapy Effects
Radiation therapy, particularly when directed at the abdominal or pelvic regions, can cause significant damage to healthy bowel tissue. The immediate effects can include inflammation and swelling, but long-term complications are more concerning. Radiation can lead to fibrosis, a process where normal tissue is replaced by scar tissue. This scar tissue is less elastic and can cause strictures (narrowing) or adhesions (bands of scar tissue that bind loops of bowel together). These changes can progressively reduce the bowel lumen or kink the bowel, leading to a chronic or delayed bowel obstruction. The risk of radiation-induced bowel obstruction can persist for years after treatment, with studies suggesting that up to 10-15% of patients receiving pelvic radiation may develop late bowel complications, including obstruction. (Source: American Society for Radiation Oncology).
Post-Surgical Complications
Abdominal surgery, a common treatment for many cancers, is a well-known risk factor for bowel obstruction cancer patients. The most frequent post-surgical cause is the formation of adhesions. Adhesions are fibrous bands of scar tissue that can form between organs or between organs and the abdominal wall, often as a result of the body’s healing response to surgical trauma. These adhesions can twist, kink, or compress segments of the bowel, leading to mechanical obstruction. The risk is particularly high after extensive surgeries or multiple abdominal operations. While adhesions can form at any time after surgery, they are a leading cause of small bowel obstruction in the general population, and this risk is amplified in cancer patients who often undergo complex abdominal procedures. Approximately 2-5% of patients undergoing abdominal surgery will develop a small bowel obstruction due to adhesions within their lifetime. (Source: World Journal of Surgery).
Functional & Motility Issues in Cancer Patients
Beyond physical blockages, cancer patients can also experience bowel obstruction due to impaired bowel function and motility. These functional obstructions, often termed ileus, are distinct from mechanical blockages but present with similar symptoms. Identifying what causes bowel obstruction with cancer in these scenarios requires understanding the systemic effects of treatments and medications.
Chemotherapy-Induced Ileus
Chemotherapy drugs, while effective in targeting cancer cells, can have systemic side effects that impact the gastrointestinal tract. Some chemotherapy agents, particularly vinca alkaloids (e.g., vincristine), can damage the nerves that control bowel muscle contractions, leading to a condition known as paralytic ileus. In this state, the bowel muscles temporarily stop working, preventing the normal propulsive movements (peristalsis) required to move food and waste. This functional paralysis results in a buildup of contents, causing distension, nausea, and vomiting, mimicking a mechanical obstruction. The severity and incidence of chemotherapy-induced ileus vary depending on the specific drug, dosage, and individual patient factors, but it remains a significant concern in oncology.
Opioid-Induced Constipation
Pain management is a critical aspect of cancer care, and opioids are frequently prescribed to alleviate severe pain. However, opioids are well-known to slow down gut motility significantly, leading to severe constipation. This condition, known as opioid-induced constipation (OIC), can progress to a functional bowel obstruction if not managed effectively. Opioids bind to receptors in the gastrointestinal tract, reducing intestinal secretions and decreasing propulsive contractions, making stool harder and more difficult to pass. While not a direct mechanical blockage, the severe impaction of stool can create a functional obstruction, requiring aggressive laxative regimens or other interventions. OIC affects a substantial number of cancer patients on chronic opioid therapy, with prevalence rates reported as high as 40-90% depending on the patient population and definition used. (Source: Journal of Pain and Symptom Management).
Other Contributing Factors & Risk Factors
Several other factors can contribute to the development of bowel obstruction in cancer patients, often acting in conjunction with tumor-related or treatment-induced causes. These additional risk factors for bowel obstruction cancer patients face can exacerbate existing conditions or independently lead to complications.
Pre-existing Adhesions
Patients who have undergone previous abdominal surgeries for conditions unrelated to their current cancer diagnosis may have pre-existing adhesions. These adhesions, formed from prior trauma or inflammation, can become problematic when combined with the effects of cancer or its treatments. For example, if a patient with pre-existing adhesions develops a new tumor or undergoes further surgery, these old adhesions can become tighter, kink the bowel, or contribute to a more complex obstructive picture. This highlights why a thorough medical history, including past surgical interventions, is crucial in assessing the overall bowel blockage reasons cancer patients might experience.
Electrolyte Imbalances
Electrolyte imbalances, particularly low levels of potassium (hypokalemia) or magnesium (hypomagnesemia), can significantly impair bowel function. These electrolytes play a vital role in muscle contraction, including the smooth muscles of the bowel. In cancer patients, electrolyte disturbances can arise from various sources, such as poor nutritional intake, vomiting, diarrhea (often chemotherapy-induced), kidney dysfunction, or certain medications. When electrolyte levels are critically low, the bowel muscles may not contract effectively, leading to reduced peristalsis and a functional ileus. Addressing and correcting these imbalances is an important part of managing and preventing functional bowel obstructions, as they are among the systemic causes of bowel obstruction in cancer patients that can be overlooked.
Frequently Asked Questions
What are the initial signs of bowel obstruction in cancer patients?
Initial signs often include persistent abdominal pain or cramping, which may be intermittent or constant. Patients might also experience nausea, vomiting (especially after eating), and a feeling of fullness or bloating. Changes in bowel habits, such as decreased stool output or inability to pass gas, are also common. Recognizing these early symptoms is crucial for prompt medical evaluation and intervention, as timely diagnosis can prevent more severe complications.
How is bowel obstruction diagnosed in cancer patients?
Diagnosis typically involves a physical examination, including assessment of abdominal distension and tenderness. Imaging studies are essential, with X-rays often showing dilated loops of bowel and air-fluid levels. Computed Tomography (CT) scans are particularly valuable, providing detailed images that can identify the location, cause (e.g., tumor, adhesions), and severity of the obstruction. Blood tests may also be performed to check for electrolyte imbalances or signs of infection.
Can bowel obstruction in cancer patients be prevented?
Complete prevention is not always possible due to the complex nature of cancer and its treatments. However, strategies can reduce the risk. These include careful surgical techniques to minimize adhesion formation, vigilant management of chemotherapy side effects, and proactive treatment of opioid-induced constipation. Regular monitoring of electrolyte levels and prompt correction of imbalances are also important. Early detection and management of underlying causes are key to mitigating the risk and severity of obstructions.