Cardiac Tamponade
Cardiac tamponade is a critical medical emergency where an excessive accumulation of fluid in the pericardial sac compresses the heart, severely impeding its ability to pump blood effectively. This life-threatening condition requires immediate medical intervention to prevent fatal outcomes.
Key Takeaways
- Cardiac tamponade is a severe condition caused by fluid buildup around the heart, restricting its function.
- It is a medical emergency requiring prompt diagnosis and treatment.
- Common Cardiac tamponade symptoms include shortness of breath, chest pain, and signs of low blood pressure.
- Causes of cardiac tamponade range from trauma and infections to cancer and medical procedures.
- The primary Cardiac tamponade treatment involves draining the fluid, typically through pericardiocentesis.
What is Cardiac Tamponade: An Overview
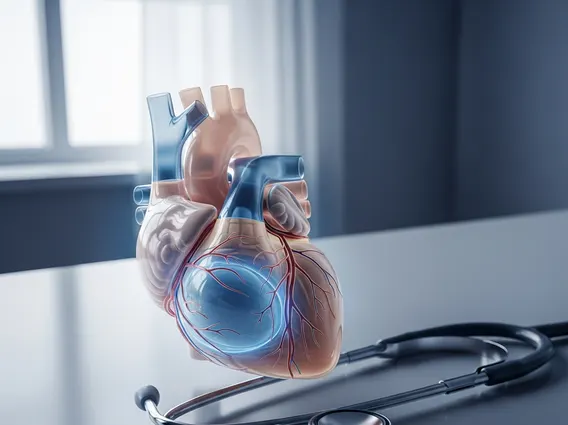
To understand what is Cardiac Tamponade, it’s essential to recognize the role of the pericardium, a double-layered sac surrounding the heart. This sac normally contains a small amount of fluid that lubricates the heart and allows it to beat without friction. Cardiac tamponade occurs when fluid—which can be blood, pus, or serous fluid—accumulates rapidly or in large volumes within this pericardial sac. This buildup exerts pressure on the heart, preventing its chambers from filling properly during diastole. As a result, the heart’s ability to pump oxygenated blood to the body is severely compromised, leading to a rapid decline in circulatory function. While relatively uncommon, it is a critical condition with a high mortality rate if not diagnosed and treated promptly, often requiring emergency care.
Cardiac Tamponade Symptoms & Underlying Causes
Recognizing Cardiac tamponade symptoms is crucial for timely intervention. Patients often present with a combination of signs reflecting reduced cardiac output and increased pressure around the heart. Common symptoms include severe shortness of breath (dyspnea), chest pain that may worsen with deep breaths, and lightheadedness or fainting due to low blood pressure. Clinically, healthcare providers may observe rapid heart rate (tachycardia), distended neck veins (jugular venous distension), and muffled heart sounds. A distinctive sign is pulsus paradoxus, an abnormally large drop in blood pressure during inhalation, indicating significant cardiac compression.
The Causes of cardiac tamponade are diverse and can stem from various medical conditions or traumatic events. Traumatic injuries to the chest, such as stab wounds or motor vehicle accidents, are frequent culprits, leading to bleeding into the pericardial sac. Medical procedures, including cardiac surgery complications, catheterizations, or pacemaker insertions, can also inadvertently cause pericardial fluid accumulation. Other causes include inflammatory conditions like acute pericarditis, certain cancers that metastasize to the pericardium, infections (bacterial, viral, or fungal), and kidney failure (uremia), which can lead to fluid retention and inflammation around the heart.
Cardiac Tamponade Treatment Options
Effective Cardiac tamponade treatment is an urgent medical priority aimed at relieving the pressure on the heart and restoring normal cardiac function. The primary and most immediate intervention is pericardiocentesis, a procedure where a needle is inserted through the chest wall into the pericardial sac to drain the excess fluid. This can be performed under ultrasound guidance to ensure safety and precision, providing rapid relief of symptoms and stabilizing the patient’s hemodynamics. In cases of recurrent tamponade, significant bleeding, or when pericardiocentesis is not feasible, surgical options such as a pericardial window (creating a small opening in the pericardium) may be considered to allow continuous drainage.
Beyond the immediate drainage, treatment also involves supportive care, which may include intravenous fluids to help maintain blood pressure and medications to support heart function. Crucially, addressing the underlying cause of the fluid accumulation is vital to prevent recurrence. This might involve treating infections with antibiotics, managing inflammatory conditions, or addressing malignancy. The prognosis largely depends on the speed of diagnosis and the effectiveness of the initial intervention, highlighting the importance of immediate medical attention for anyone suspected of having cardiac tamponade.
