Breast Columnar Cell Lesion
Breast columnar cell lesion refers to a group of benign changes found in the breast tissue, characterized by alterations in the cells lining the breast ducts. Understanding these cellular alterations is crucial for both patients and healthcare providers in managing breast health, as they are frequently encountered in breast biopsies.
Key Takeaways
- A breast columnar cell lesion involves changes where cells lining breast ducts become taller and more columnar, typically considered benign.
- These lesions are usually asymptomatic, meaning there are no noticeable breast columnar cell lesion symptoms, and they are often discovered incidentally during imaging.
- Diagnosis relies on imaging techniques, primarily mammography for detecting microcalcifications, followed by a biopsy for definitive tissue analysis.
- Pathological examination is key to understanding the specific breast columnar cell changes explained, differentiating between benign forms and those with atypia.
- While generally benign, lesions with atypia may warrant closer monitoring due to a slightly increased association with other proliferative breast conditions, making accurate breast columnar cell lesion diagnosis vital.
What is Breast Columnar Cell Lesion?
A breast columnar cell lesion represents a common, usually benign finding in breast tissue, characterized by the presence of cells that are taller and more columnar than typical, lining the terminal duct-lobular units. These microscopic changes are often discovered incidentally during biopsies performed to investigate other findings, such as microcalcifications detected on a mammogram. They are considered part of the spectrum of benign breast conditions.
The classification of breast columnar cell changes explained ranges from simple columnar cell change (CCC) or columnar cell hyperplasia (CCH) without atypia, to columnar cell change with atypia (CCA), also known as atypical columnar cell lesion. While the majority of columnar cell lesions are entirely benign and do not increase breast cancer risk, those with atypia are recognized to have a slightly increased association with other proliferative lesions, including ductal carcinoma in situ (DCIS), or a modest increase in future breast cancer risk. This distinction is critical for guiding patient management and follow-up, as highlighted by guidelines from organizations like the American College of Surgeons.
Symptoms of Breast Columnar Cell Lesion
Typically, breast columnar cell lesion symptoms are absent, meaning these lesions do not cause noticeable physical signs or discomfort. Patients usually do not experience palpable lumps, breast pain, nipple discharge, or skin changes directly attributable to columnar cell lesions. This asymptomatic nature means that their detection is almost always incidental, occurring during routine breast screening or diagnostic work-ups for other breast concerns.
The most common way these lesions are identified is through the presence of microcalcifications on a mammogram. These tiny calcium deposits are not symptoms felt by the patient but are radiological findings that can prompt further investigation. While microcalcifications can be associated with various breast conditions, including benign and malignant ones, their presence often leads to a biopsy where columnar cell lesions may be discovered. It is important for individuals to continue with regular breast screenings, as these can detect subtle changes before any symptoms arise.
Diagnosing Breast Columnar Cell Changes
The accurate breast columnar cell lesion diagnosis relies on a systematic approach involving both advanced imaging techniques and definitive tissue analysis. Given that these lesions are typically asymptomatic, their discovery often follows the detection of subtle changes during routine breast health screenings.
Imaging Techniques
The initial step in identifying potential columnar cell changes frequently involves mammography. This imaging modality is highly effective at detecting microcalcifications, which are often the primary indicator of these lesions. These calcifications appear as small, sometimes clustered, white spots on the mammogram. While microcalcifications are common and often benign, their presence warrants further investigation. Other imaging methods, such as ultrasound or magnetic resonance imaging (MRI), may be employed to further evaluate any associated masses or areas of concern, though columnar cell lesions themselves are rarely visible as distinct masses unless they are part of a larger, more complex lesion.
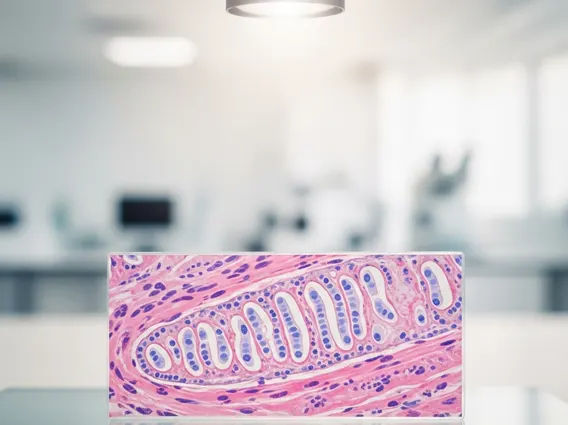
Biopsy and Pathology
For a definitive diagnosis, a biopsy is essential to obtain tissue samples from the suspicious area. This procedure can be performed using a core needle biopsy, which extracts small cylinders of tissue, or an excisional biopsy, which removes the entire area of concern. The collected tissue is then meticulously examined by a pathologist under a microscope. This detailed pathological assessment is crucial for identifying the characteristic breast columnar cell changes explained, including the specific cellular architecture and the presence or absence of atypia. The pathologist’s report provides the definitive diagnosis, guiding subsequent management decisions, which may range from routine follow-up to further intervention, depending on the lesion’s specific characteristics.
