Breast Carcinoma In Situ
Breast carcinoma in situ represents an early form of breast cancer where abnormal cells are confined to the milk ducts or lobules. Understanding this condition is crucial for early detection and effective management, preventing its potential progression.
Key Takeaways
- Breast Carcinoma In Situ (BCIS) involves abnormal cells confined within breast ducts or lobules, not yet spread.
- It is often asymptomatic and typically detected through routine mammography.
- Ductal Carcinoma In Situ (DCIS) is the most common type, distinct from invasive cancer where cells have broken through the duct walls.
- Treatment options vary but often include surgery (lumpectomy or mastectomy), sometimes followed by radiation therapy or hormonal therapy.
- Early diagnosis and appropriate intervention are key to preventing progression to invasive breast cancer.
What is Breast Carcinoma In Situ?
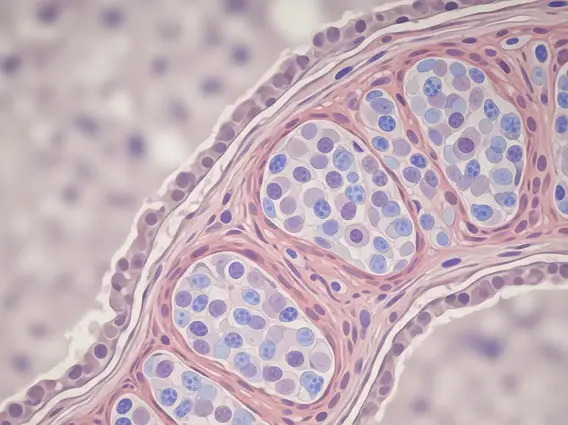
Breast Carcinoma In Situ (BCIS) refers to a non-invasive condition where abnormal cells are present within the breast but have not spread beyond their original location. Specifically, these cells are contained within the milk ducts or lobules of the breast, meaning they have not invaded the surrounding breast tissue. This early stage is considered “in situ” because the carcinoma is “in its original place.” While not yet invasive cancer, BCIS is considered a precursor to invasive breast cancer, highlighting the importance of timely diagnosis and management. The most common form of BCIS is Ductal Carcinoma In Situ (DCIS), found in the milk ducts, which is what is breast carcinoma in situ primarily refers to in clinical practice.
Ductal Carcinoma In Situ vs. Invasive Cancer
Understanding the distinction between ductal carcinoma in situ vs invasive cancer is fundamental. In ductal carcinoma in situ (DCIS), the abnormal cells are entirely contained within the lining of the milk ducts and have not broken through the duct walls into the surrounding stromal tissue. This means DCIS has no potential to metastasize (spread to other parts of the body) because it lacks access to blood vessels and lymphatic channels. In contrast, invasive breast cancer occurs when cancerous cells have breached the duct or lobule walls and infiltrated the surrounding breast tissue. Once invasive, these cells gain access to the bloodstream and lymphatic system, enabling them to potentially spread to distant organs. According to the American Cancer Society, DCIS accounts for about 20% of all newly diagnosed breast cancers in the United States, emphasizing its prevalence as a non-invasive form.
Recognizing Symptoms and Diagnosis
One of the defining characteristics of breast carcinoma in situ symptoms is their frequent absence. Most individuals with BCIS, particularly DCIS, do not experience any noticeable signs or symptoms. This makes routine screening a critical tool for detection. When symptoms do occur, they are often subtle and non-specific, such as a small lump that can be felt, nipple discharge, or changes in the skin of the breast. However, these are rare for BCIS and more commonly associated with other breast conditions or invasive cancer.
The primary method for diagnosing BCIS is through a mammogram. Calcifications, which are tiny specks of calcium, are often the only sign of DCIS on a mammogram. If suspicious calcifications or other abnormalities are identified, further diagnostic steps are taken. These typically include:
- Diagnostic Mammogram: Provides more detailed images of the suspicious area.
- Ultrasound: Used to assess if the area is solid or fluid-filled.
- Biopsy: A definitive diagnosis requires a tissue sample (core needle biopsy or surgical biopsy) to be examined under a microscope by a pathologist. This confirms the presence of abnormal cells and whether they are confined to the ducts or lobules.
Breast Carcinoma In Situ Treatment Options
The goal of breast carcinoma in situ treatment options is to remove the abnormal cells and prevent their progression to invasive cancer. Treatment plans are highly individualized, considering factors such as the size and grade of the DCIS, the patient’s age, and personal preferences.
Common treatment approaches include:
- Surgery:
- Lumpectomy (Breast-Conserving Surgery): This involves removing only the area of DCIS and a small margin of healthy tissue around it. It is often followed by radiation therapy.
- Mastectomy: In some cases, particularly for large areas of DCIS, multiple areas of DCIS, or if radiation therapy is not an option, a total mastectomy (removal of the entire breast) may be recommended.
- Radiation Therapy: Often recommended after a lumpectomy to destroy any remaining abnormal cells and reduce the risk of recurrence in the treated breast.
- Hormonal Therapy: For DCIS that is hormone receptor-positive, medications like tamoxifen or aromatase inhibitors may be prescribed. These therapies block the effects of estrogen, which can fuel the growth of some breast cancer cells, thereby reducing the risk of recurrence or developing a new breast cancer in either breast. This is typically an adjuvant therapy, meaning it’s given after primary treatment.
The choice of treatment is a shared decision between the patient and their medical team, aiming for the most effective outcome with the least impact on quality of life.