Posterior Reversible Encephalopathy Syndrome
Posterior Reversible Encephalopathy Syndrome (PRES) is a complex neurological disorder characterized by a sudden onset of symptoms and specific brain imaging findings. It is often associated with various underlying medical conditions, leading to temporary brain dysfunction.
Key Takeaways
- PRES is an acute neurological condition primarily affecting the posterior regions of the brain.
- It is characterized by symptoms such as headache, seizures, visual disturbances, and altered mental status.
- Common causes include severe hypertension, kidney failure, certain autoimmune diseases, and immunosuppressive medications.
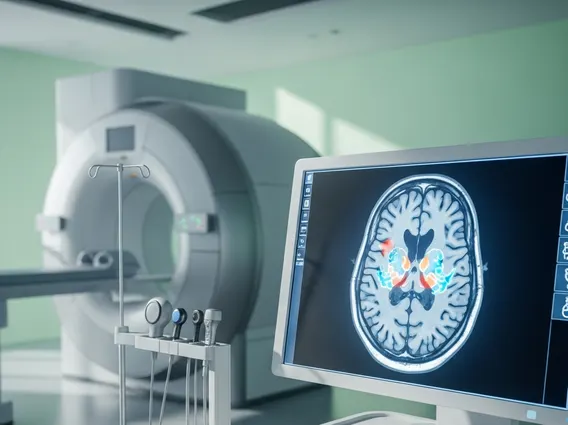
- Diagnosis relies on clinical presentation and characteristic findings on brain imaging, typically MRI.
- Treatment focuses on managing the underlying cause, and with prompt intervention, the condition is often reversible.
What is Posterior Reversible Encephalopathy Syndrome (PRES)?
Posterior Reversible Encephalopathy Syndrome explained refers to an acute neurological disorder characterized by a constellation of symptoms and distinctive neuroimaging findings. It is also known as a reversible posterior leukoencephalopathy syndrome. This condition primarily affects the posterior (back) regions of the brain, although other areas can also be involved. The hallmark of PRES is vasogenic edema, which means fluid leakage from blood vessels into the brain tissue, rather than cell death.
While the exact incidence of PRES is not precisely known due to its varied presentation and underlying causes, it is considered a rare but increasingly recognized condition, particularly in critical care settings. It can affect individuals of all ages, though it is more frequently observed in adults. The “reversible” aspect of the syndrome highlights that, with timely and appropriate management of the underlying triggers, most patients experience a full recovery of their neurological function and resolution of brain imaging abnormalities.
Symptoms and Causes of PRES
The clinical presentation of PRES can vary widely among individuals, but several key symptoms are commonly observed. Recognizing these signs is crucial for early diagnosis and intervention. The collective term PRES syndrome symptoms and causes encompasses a range of neurological manifestations and predisposing conditions.
Common symptoms of PRES include:
- Headache: Often severe and sudden in onset.
- Seizures: Ranging from focal to generalized tonic-clonic seizures, occurring in a significant number of patients.
- Visual disturbances: Such as blurred vision, hemianopsia (loss of half of the visual field), or even cortical blindness (inability to see despite healthy eyes).
- Altered mental status: Including confusion, lethargy, drowsiness, or even coma.
- Nausea and vomiting: Often accompanying severe headache.
PRES is not a disease in itself but rather a syndrome triggered by various underlying conditions that disrupt cerebral autoregulation and endothelial function. The most common cause is acute, severe hypertension, where a sudden spike in blood pressure overwhelms the brain’s ability to regulate blood flow, leading to vasogenic edema. Other significant causes include:
| Category | Specific Conditions/Factors |
|---|---|
| Hypertensive Disorders | Preeclampsia, eclampsia, hypertensive crisis, pheochromocytoma |
| Renal Disease | Acute or chronic kidney failure, hemodialysis |
| Autoimmune Diseases | Systemic lupus erythematosus (SLE), vasculitis, scleroderma |
| Immunosuppressive Therapy | Cyclosporine, tacrolimus, cisplatin, interferon-alpha |
| Sepsis and Shock | Severe infections, septic shock |
Understanding these diverse triggers is essential for identifying individuals at risk and guiding targeted therapeutic strategies.
Managing PRES: Treatment and Prognosis
Effective management of PRES hinges on prompt diagnosis and aggressive treatment of the underlying cause. The primary goal is to stabilize the patient’s condition, alleviate symptoms, and prevent further neurological damage. Reversible encephalopathy treatment options primarily focus on addressing the precipitating factors.
For patients with severe hypertension, careful and controlled reduction of blood pressure is paramount to prevent further edema and potential complications like intracranial hemorrhage. Antihypertensive medications are administered intravenously to achieve a gradual decrease in blood pressure, typically by 15-25% within the first hour. Seizures, if present, are managed with antiepileptic drugs, which may be continued for a short period after the acute phase, depending on the patient’s recovery and risk factors.
In cases where PRES is linked to specific medications, such as immunosuppressants, dose reduction or discontinuation of the offending agent may be necessary, often in consultation with the prescribing specialist. For other underlying conditions like kidney failure or autoimmune diseases, managing these primary illnesses is crucial for the resolution of PRES. Most patients with PRES experience a favorable prognosis, with symptoms resolving and brain imaging abnormalities disappearing within days to weeks, especially with early and appropriate treatment. However, a small percentage of patients may experience residual neurological deficits or recurrence, particularly if the underlying cause is not fully controlled or if there were severe complications during the acute phase.