Portal Hypertension
Portal Hypertension is a serious medical condition characterized by abnormally high blood pressure within the portal vein system, which carries blood from the digestive organs to the liver. This elevated pressure can lead to severe complications affecting multiple bodily systems.
Key Takeaways
- Portal Hypertension involves increased pressure in the portal vein, often due to resistance to blood flow in the liver.
- The most common cause is cirrhosis, leading to scarring that obstructs blood flow.
- Symptoms can include fluid accumulation (ascites), enlarged spleen, and gastrointestinal bleeding from varices.
- Diagnosis typically involves imaging, endoscopy, and sometimes liver biopsy.
- Treatment focuses on managing complications and lowering portal pressure, often through medication, endoscopic procedures, or shunts.
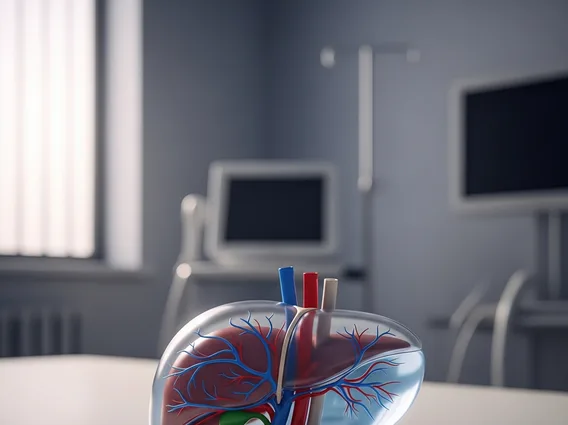
What is Portal Hypertension?
Portal Hypertension refers to a condition where there is an increase in blood pressure within the portal venous system. This system is a critical network of veins that transports blood from the stomach, intestines, spleen, and pancreas directly to the liver. When blood flow through the liver is obstructed, typically due to scarring or blockages, pressure builds up in these veins, leading to portal hypertension.
This elevated pressure can force blood to reroute through smaller, more fragile veins, which can then become enlarged and prone to bleeding. The liver plays a vital role in filtering toxins and processing nutrients, and when its function is compromised by conditions leading to portal hypertension, systemic health can be significantly impacted.
Symptoms and Causes of Portal Hypertension
The manifestation of portal hypertension symptoms causes varies depending on the severity and underlying cause. Many individuals may not experience noticeable symptoms until complications arise. Common symptoms often include:
- Ascites: Accumulation of fluid in the abdomen, leading to swelling and discomfort.
- Gastrointestinal Bleeding: Caused by ruptured varices (enlarged veins) in the esophagus or stomach, which can manifest as black, tarry stools (melena) or vomiting blood (hematemesis).
- Encephalopathy: Confusion, disorientation, or forgetfulness due to toxins building up in the bloodstream that the liver cannot adequately filter.
- Splenomegaly: Enlargement of the spleen, which can lead to a decrease in blood cell counts.
The primary cause of portal hypertension is cirrhosis, a condition where healthy liver tissue is replaced by scar tissue, impeding blood flow. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), cirrhosis affects approximately 1 in 400 adults in the United States, with portal hypertension being a common complication. Other causes can include blood clots in the portal vein (portal vein thrombosis), certain parasitic infections like schistosomiasis, or rare conditions affecting the liver’s blood vessels.
Diagnosing and Treating Portal Hypertension
Effective management begins with accurately diagnosing portal hypertension. Diagnostic methods typically involve a combination of clinical evaluation, imaging studies, and sometimes invasive procedures. Imaging techniques such as ultrasound, CT scans, and MRI can visualize the portal vein and assess liver damage. Endoscopy, a procedure where a thin, flexible tube with a camera is inserted into the esophagus and stomach, is crucial for detecting and evaluating esophageal and gastric varices. In some cases, a liver biopsy may be performed to determine the extent of liver damage and the underlying cause.
Once diagnosed, portal hypertension treatment options focus on managing its complications and reducing portal pressure. Treatment strategies include:
- Medications: Beta-blockers are often prescribed to lower blood pressure in the portal system and reduce the risk of variceal bleeding. Diuretics may be used to manage ascites.
- Endoscopic Therapy: Procedures like variceal banding (ligation) or sclerotherapy can be performed during an endoscopy to prevent or stop bleeding from varices.
- Shunt Procedures: In severe cases, surgical or radiological shunts (e.g., Transjugular Intrahepatic Portosystemic Shunt or TIPS) may be created to reroute blood flow and reduce pressure in the portal vein.
- Liver Transplant: For individuals with end-stage liver disease and severe portal hypertension, a liver transplant may be the definitive treatment.
Ongoing monitoring and a multidisciplinary approach are essential for individuals with portal hypertension to prevent complications and improve quality of life.