Perivascular Epithelioid Cell Tumor
Perivascular Epithelioid Cell Tumor (PEComa) is a rare group of mesenchymal tumors characterized by their unique cellular features and specific immunohistochemical markers. These tumors can arise in various organs throughout the body, presenting a diagnostic challenge due to their diverse manifestations.
Key Takeaways
- Perivascular Epithelioid Cell Tumor (PEComa) is a rare mesenchymal tumor that can appear in many organs.
- Symptoms are highly variable, depending on the tumor’s location and size, often discovered incidentally.
- Diagnosis relies on imaging, biopsy, and specific immunohistochemical staining.
- Treatment primarily involves surgical removal, with targeted therapies considered for advanced or unresectable cases.
- PEComas range from benign to malignant, requiring careful evaluation and follow-up.
What is Perivascular Epithelioid Cell Tumor?
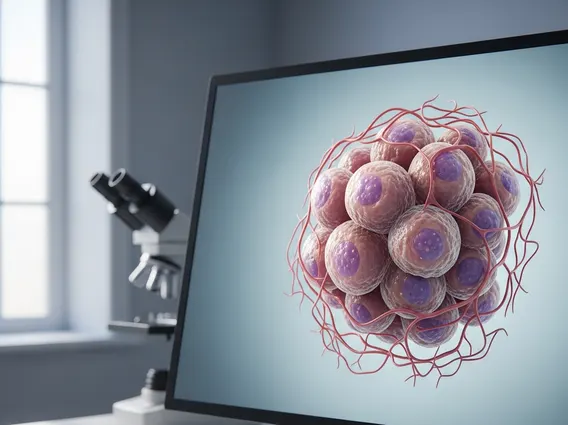
Perivascular Epithelioid Cell Tumor (PEComa) refers to a distinct family of mesenchymal tumors composed of histologically and immunohistochemically distinctive perivascular epithelioid cells. These cells typically co-express melanocytic markers (like HMB-45, Melan-A) and muscle markers (like smooth muscle actin). PEComas are considered rare, with their exact incidence not fully established due to their varied presentation and classification challenges. They can occur in virtually any anatomical site, including the uterus, kidney, liver, lung, and soft tissues, though the uterus and kidney are among the more common locations. While many PEComas are benign, some exhibit malignant features, necessitating careful pathological assessment to determine their biological potential.
The precise origin of perivascular epithelioid cells is still a subject of ongoing research, but they are thought to be related to smooth muscle cells or melanocytes. Their characteristic perivascular growth pattern, where tumor cells are arranged around blood vessels, is a defining feature. The clinical behavior of PEComas can range from indolent to aggressive, making accurate diagnosis and risk stratification crucial for patient management.
Symptoms and Diagnosis of Perivascular Epithelioid Cell Tumor
The presentation of perivascular epithelioid cell tumor symptoms is highly variable and largely dependent on the tumor’s location, size, and whether it is compressing surrounding structures. Many PEComas are discovered incidentally during imaging studies performed for other reasons, especially when they are small and asymptomatic. When symptoms do occur, they can be non-specific and mimic other conditions. For instance, a PEComa in the uterus might cause abnormal uterine bleeding or pelvic pain, while a renal PEComa could lead to flank pain or hematuria (blood in urine). Larger tumors, regardless of location, may cause a palpable mass or symptoms related to mass effect, such as abdominal discomfort or bowel obstruction.
The perivascular epithelioid cell tumor diagnosis typically involves a multi-step process. Initial detection often occurs through imaging techniques such as ultrasound, CT scans, or MRI, which can identify a mass. However, these imaging studies cannot definitively diagnose a PEComa, as its appearance can overlap with other tumor types. A definitive diagnosis requires a tissue biopsy, where a small sample of the tumor is removed and examined under a microscope by a pathologist. Immunohistochemical staining is critical in this process, as the co-expression of melanocytic and muscle markers is a hallmark of PEComas. Genetic testing may also be performed, particularly to look for mutations in the TSC1 or TSC2 genes, which are associated with tuberous sclerosis complex and can predispose individuals to PEComas.
- Common Symptom Indicators:
- Abdominal or flank pain
- Palpable mass
- Abnormal bleeding (e.g., uterine)
- Fatigue or weight loss (in advanced cases)
- Symptoms related to organ dysfunction (e.g., kidney failure, liver issues)
Treatment Options for Perivascular Epithelioid Cell Tumor
The primary perivascular epithelioid cell tumor treatment is surgical resection, aiming for complete removal of the tumor whenever feasible. For benign or low-grade PEComas, complete surgical excision is often curative. The extent of surgery depends on the tumor’s size, location, and proximity to vital structures. In cases where the tumor is large, multifocal, or located in a challenging anatomical site, a multidisciplinary team approach involving various surgical specialists may be necessary.
For malignant or unresectable PEComas, or those that have metastasized, other treatment modalities may be considered. These can include systemic therapies, such as mTOR inhibitors (e.g., sirolimus, everolimus). These drugs target the mTOR pathway, which is often dysregulated in PEComas, particularly those associated with tuberous sclerosis complex. Radiation therapy may also be used in specific situations, such as for local control of unresectable tumors or to manage symptoms. Chemotherapy has generally shown limited efficacy in PEComas compared to targeted therapies. Given the rarity and variability of these tumors, treatment plans are highly individualized, often guided by the tumor’s specific characteristics, the patient’s overall health, and expert consultation from specialized oncology centers.