Percutaneous
Percutaneous procedures represent a significant advancement in modern medicine, offering less invasive alternatives to traditional surgical techniques. This approach has transformed patient care across numerous specialties by minimizing trauma, reducing recovery times, and improving overall patient outcomes.

Key Takeaways
- Percutaneous procedures involve accessing internal organs or tissues through the skin using needles or small incisions.
- These minimally invasive techniques often result in reduced pain, smaller scars, and faster recovery times compared to open surgery.
- Common percutaneous medical procedures include angioplasty, biopsies, and certain pain management interventions, widely used in various medical fields.
- A key distinction lies in percutaneous vs open surgery, with the former emphasizing minimal disruption to the body’s tissues.
What is Percutaneous?
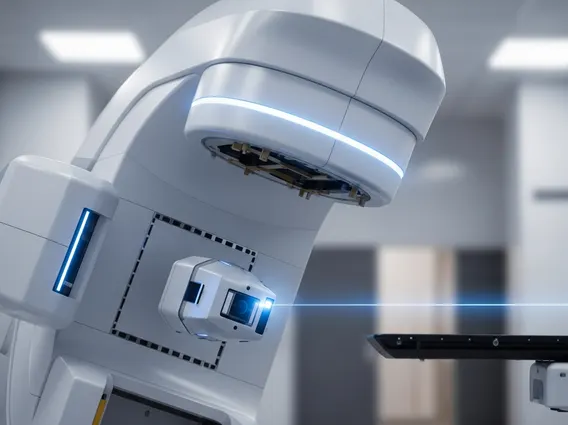
Percutaneous refers to medical procedures performed through the skin, typically involving a small puncture or incision rather than a large surgical opening. This approach allows physicians to access internal structures, such as blood vessels, organs, or tissues, with minimal disruption to surrounding healthy tissue. The percutaneous definition emphasizes the “through the skin” aspect, distinguishing it from more invasive surgical methods that require extensive incisions. These techniques often utilize advanced imaging guidance, such as fluoroscopy, ultrasound, or computed tomography (CT) scans, to accurately navigate specialized instruments to the target area. This precision helps to enhance both the safety and effectiveness of the procedure while significantly reducing patient discomfort and potential complications associated with larger incisions. The goal is to achieve therapeutic or diagnostic results with the least possible physical impact on the patient.
Common Percutaneous Medical Procedures
A wide array of medical interventions fall under the umbrella of percutaneous medical procedures, revolutionizing treatment across various specialties. These procedures are frequently employed in cardiology, interventional radiology, pain management, and oncology due to their less invasive nature and favorable patient outcomes. For instance, percutaneous coronary intervention (PCI), commonly known as angioplasty with stent placement, is a widely performed procedure to open blocked arteries in the heart. According to the American Heart Association, over 900,000 PCIs are performed annually in the United States, highlighting their prevalence and importance in managing cardiovascular disease and improving patient prognosis.
Other common examples of these minimally invasive techniques include:
- Percutaneous biopsies: These procedures involve obtaining tissue samples from organs like the liver, kidney, or lung for diagnostic purposes, often guided by real-time imaging to ensure accuracy.
- Percutaneous nephrolithotomy (PCNL): A highly effective procedure for removing large kidney stones through a small incision in the back, offering a less invasive alternative to open surgery for complex stones.
- Percutaneous vertebroplasty and kyphoplasty: These are treatments for spinal compression fractures, involving the injection of bone cement into fractured vertebrae to stabilize them and alleviate pain.
- Percutaneous drainage: This technique is used to remove abnormal fluid collections, such as abscesses, cysts, or effusions, from various body parts, often guided by ultrasound or CT.
These procedures consistently lead to shorter hospital stays, reduced recovery times, and quicker returns to daily activities for patients, significantly improving their quality of life post-intervention.
Percutaneous vs. Open Surgery: Key Differences
The fundamental distinction between percutaneous vs open surgery lies in the extent of bodily invasion and the approach to accessing the surgical site. Open surgery involves making a large incision to directly visualize and operate on internal organs, requiring significant tissue dissection and manipulation. In contrast, percutaneous procedures utilize small punctures or incisions, often less than a centimeter, relying on specialized instruments and real-time imaging for precise guidance. This difference has profound implications for patient recovery, post-operative pain, and overall outcomes. The minimally invasive nature of percutaneous techniques aims to preserve surrounding healthy tissues, leading to a host of benefits.
Here’s a comparison of key differences that highlight why percutaneous approaches are often preferred when clinically appropriate:
| Feature | Percutaneous Procedures | Open Surgery |
|---|---|---|
| Incision Size | Small puncture or incision (typically <1 cm) | Large incision (several centimeters to inches) |
| Tissue Disruption | Minimal, preserving surrounding healthy tissue | Significant, requiring extensive dissection |
| Post-operative Pain | Generally lower due to less tissue trauma | Generally higher, often requiring stronger pain management |
| Recovery Time | Often shorter, allowing faster return to normal activities | Typically longer, with extended hospital stays and rehabilitation |
| Scarring | Minimal, often barely noticeable cosmetic result | More prominent and visible scars |
| Anesthesia | Local anesthesia with sedation often sufficient; general anesthesia also used | Usually requires general anesthesia |
Patients undergoing percutaneous interventions typically experience less post-operative pain, a reduced risk of infection, and a quicker overall recovery compared to those undergoing traditional open surgery. This makes percutaneous techniques a highly valued and often preferred option when clinically appropriate, contributing significantly to improved patient satisfaction and healthcare efficiency.