Parathyroidectomy
Parathyroidectomy is a surgical procedure involving the removal of one or more parathyroid glands, which are small glands located in the neck near the thyroid. This operation is primarily performed to treat conditions caused by overactive parathyroid glands.
Key Takeaways
- Parathyroidectomy is a surgical intervention to remove overactive parathyroid glands, typically addressing hyperparathyroidism.
- The main reason for this operation is primary hyperparathyroidism, characterized by excessive parathyroid hormone leading to high blood calcium levels.
- Symptoms necessitating surgery can include kidney stones, bone density loss, fatigue, and cognitive issues.
- The procedure can be minimally invasive, leading to a relatively quick recovery, though calcium monitoring is crucial afterward.
- Patients generally experience significant improvement in symptoms and quality of life following successful parathyroidectomy.
What is Parathyroidectomy?
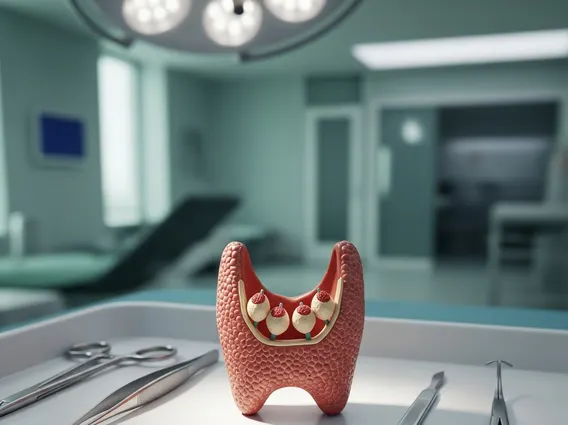
Parathyroidectomy is a surgical procedure to remove one or more of the four parathyroid glands. These pea-sized glands, located in the neck behind the thyroid, play a crucial role in regulating calcium and phosphorus levels in the body by producing parathyroid hormone (PTH). The surgery is performed when one or more of these glands become overactive, leading to a condition known as hyperparathyroidism.
The primary goal of parathyroidectomy surgery is to normalize blood calcium levels, thereby alleviating symptoms and preventing long-term complications associated with persistently high calcium. The extent of the surgery can vary, from removing a single adenoma (a benign tumor on one gland) to removing multiple glands or even a portion of the thyroid if necessary, depending on the underlying cause of hyperparathyroidism.
Reasons for Parathyroidectomy Operation
The most common reason for a parathyroidectomy operation is primary hyperparathyroidism (PHPT), a condition where one or more parathyroid glands produce too much parathyroid hormone independently. This excess hormone leads to elevated calcium levels in the blood (hypercalcemia), which can have widespread effects on the body. While some individuals with PHPT may be asymptomatic, many experience significant health issues.
Indications for surgery typically include:
- Significant elevation of blood calcium levels.
- Reduced bone mineral density, leading to osteoporosis or osteopenia.
- Kidney stones or nephrocalcinosis (calcium deposits in the kidneys).
- Impaired kidney function, even if mild.
- Neuromuscular symptoms such as fatigue, weakness, or difficulty concentrating.
- Age under 50, even with mild hypercalcemia, due to the long-term risk of complications.
Less common reasons for parathyroidectomy include secondary hyperparathyroidism (often seen in patients with chronic kidney disease) and tertiary hyperparathyroidism, where the glands become autonomous after prolonged secondary stimulation. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), primary hyperparathyroidism affects approximately 100,000 people in the United States each year, with surgery being the only definitive cure.
The Parathyroidectomy Procedure: Recovery and Life After
The Parathyroidectomy procedure and recovery vary depending on the surgical approach. Modern techniques often involve minimally invasive parathyroidectomy (MIP), which uses smaller incisions and targeted removal of the affected gland(s) after precise localization. This can lead to shorter hospital stays, less pain, and quicker recovery compared to traditional open surgery, which involves a larger incision and exploration of all four glands.
Patients typically spend one night in the hospital, though some minimally invasive procedures allow for same-day discharge. Recovery usually involves managing mild pain or discomfort with over-the-counter medication. Most individuals can resume light activities within a few days and return to normal activities within one to two weeks. Post-operative care includes monitoring blood calcium levels, as a temporary drop (hypocalcemia) can occur, sometimes requiring calcium and vitamin D supplementation.
Life after parathyroidectomy generally sees a significant improvement in symptoms and overall quality of life. Bone density may improve, the risk of kidney stones decreases, and many patients report increased energy and better cognitive function. Long-term follow-up involves periodic blood tests to ensure calcium and PTH levels remain within a healthy range. While the surgery is highly effective, it’s essential for patients to adhere to their doctor’s recommendations for monitoring and any necessary supplementation to maintain optimal health.