Padcev
Padcev (enfortumab vedotin-ejfv) is a targeted therapy representing a significant advancement in oncology. It is specifically designed to treat certain types of cancer by delivering a potent chemotherapy agent directly to cancer cells, thereby minimizing damage to healthy tissues.
Key Takeaways
- Padcev (enfortumab vedotin-ejfv) is an antibody-drug conjugate (ADC) approved for specific types of urothelial cancer.
- It works by targeting Nectin-4, a protein highly expressed on cancer cells, delivering a cytotoxic agent directly.
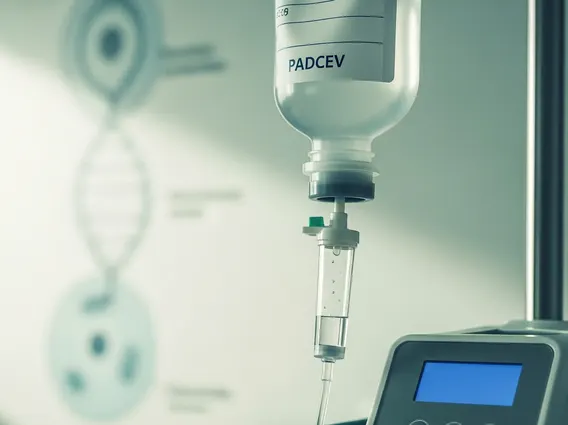
- Treatment involves intravenous infusions administered on a defined schedule, typically in cycles.
- Common side effects include skin reactions, fatigue, and peripheral neuropathy, while key benefits include improved response rates and survival outcomes.
- This targeted approach aims to enhance efficacy while potentially reducing systemic toxicity compared to conventional chemotherapy.
What is Padcev: Purpose and Mechanism of Action
Padcev is an antibody-drug conjugate (ADC) that has been approved for the treatment of adults with locally advanced or metastatic urothelial cancer, particularly after prior treatments. Urothelial cancer, which primarily affects the bladder, is the ninth most common cancer worldwide, with approximately 573,000 new cases diagnosed globally in 2020, according to the World Health Organization (WHO). The purpose of Padcev is to provide a targeted therapeutic option for patients whose disease has progressed despite other treatments.
The way Padcev works involves a sophisticated mechanism. It consists of an antibody linked to a chemotherapy drug called monomethyl auristatin E (MMAE). The antibody component specifically binds to Nectin-4, a protein that is highly expressed on the surface of many urothelial cancer cells. Once bound, Padcev is internalized by the cancer cell. Inside the cell, the MMAE chemotherapy agent is released, disrupting the cell’s microtubule network and leading to programmed cell death. This targeted delivery helps concentrate the chemotherapy agent within cancer cells, aiming to reduce systemic exposure and associated side effects compared to traditional chemotherapy.
Padcev Treatment Information and Administration
Padcev treatment information typically involves intravenous (IV) administration in an outpatient setting. The specific dosing schedule can vary but commonly involves infusions on specific days within a 21-day cycle. For example, patients might receive Padcev on Day 1, Day 8, and Day 15 of a 28-day cycle, followed by a rest period. The duration of treatment depends on the patient’s response and tolerance to the medication.
Before initiating Padcev, healthcare providers will assess a patient’s overall health, including blood counts, liver function, and blood sugar levels. During treatment, patients are closely monitored for potential adverse reactions, and dose adjustments may be necessary based on the severity of any side effects. Patients are advised to report any new or worsening symptoms promptly to their care team. Adherence to the prescribed schedule and regular monitoring are crucial for optimizing the effectiveness and safety of Padcev treatment.
Padcev Side Effects and Benefits
Like all cancer treatments, Padcev side effects and benefits must be carefully weighed. The benefits of Padcev include significant improvements in objective response rates, progression-free survival, and overall survival for patients with advanced urothelial cancer who have limited treatment options. Clinical trials have demonstrated its efficacy in patients previously treated with platinum-containing chemotherapy and PD-1/L1 inhibitors, offering a new avenue for disease control.
However, Padcev can also cause various side effects. Common side effects often include:
- Skin reactions (rash, itching, dry skin)
- Fatigue
- Peripheral neuropathy (numbness, tingling in hands or feet)
- Hyperglycemia (high blood sugar)
- Nausea and diarrhea
- Decreased appetite
- Hair loss
More serious side effects, though less common, can include severe skin reactions (some requiring hospitalization), pneumonitis (inflammation of the lungs), and severe hyperglycemia, particularly in patients with pre-existing diabetes. Patients are closely monitored for these and other potential adverse events throughout their treatment course. Managing side effects proactively is a key component of care to ensure patients can continue treatment effectively.