Oral Epithelial Dysplasia
Oral Epithelial Dysplasia represents a significant clinical finding in oral pathology, indicating abnormal changes in the cells lining the mouth. Understanding this condition is crucial for early detection and intervention to prevent potential progression to oral cancer.
Key Takeaways
- Oral Epithelial Dysplasia (OED) is a precancerous condition characterized by abnormal cell changes in the oral mucosa.
- It is classified into mild, moderate, and severe grades, reflecting the extent of cellular abnormality.
- Common symptoms include persistent white (leukoplakia) or red (erythroplakia) patches that do not resolve.
- Major risk factors include tobacco use, alcohol consumption, and human papillomavirus (HPV) infection.
- Treatment typically involves surgical removal of the affected tissue, followed by vigilant monitoring to prevent recurrence or progression.
What is Oral Epithelial Dysplasia?
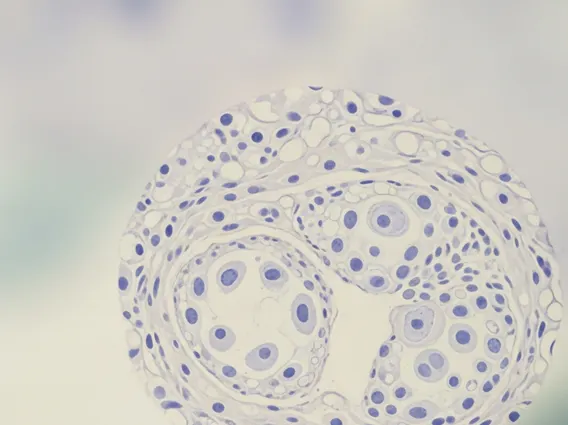
Oral Epithelial Dysplasia (OED) refers to a spectrum of architectural and cytological changes within the squamous epithelium of the oral cavity that are considered precancerous. These changes indicate an increased risk of developing squamous cell carcinoma, the most common type of oral cancer. OED is not cancer itself but rather a warning sign, signifying cellular abnormalities that have the potential to transform into malignancy over time.
The severity of oral epithelial dysplasia is typically graded based on the extent of cellular disorganization and atypical features observed under a microscope. These grades include mild, moderate, and severe dysplasia, with severe dysplasia carrying the highest risk of malignant transformation. Early identification and management of OED are paramount in preventing the progression to invasive oral cancer. According to the World Health Organization (WHO), oral cancer is a significant global health concern, and recognizing precancerous lesions like OED is a critical step in improving patient outcomes through timely intervention.
Symptoms and Causes of Oral Epithelial Dysplasia
Recognizing the signs of oral epithelial dysplasia is crucial for early diagnosis. The condition often presents with visible changes in the oral mucosa, which may be asymptomatic in its early stages. However, certain persistent lesions should prompt a medical evaluation. The primary **oral epithelial dysplasia symptoms** include:
- White Patches (Leukoplakia): These are often flat or slightly raised, firm, and cannot be scraped off. They are the most common presentation of OED.
- Red Patches (Erythroplakia): These appear as velvety, bright red areas and are less common than leukoplakia but carry a higher risk of dysplasia or malignancy.
- Mixed Red and White Patches (Erythroleukoplakia): A combination of both red and white lesions, also indicating a higher risk.
- Non-Healing Sores: Any persistent sore or ulcer in the mouth that does not heal within two weeks warrants investigation.
- Changes in Texture: The affected area might feel rough, thickened, or hardened to the touch.
The **causes of oral epithelial dysplasia** are primarily linked to chronic irritation and exposure to carcinogens. While a definitive single cause is often hard to pinpoint, several well-established risk factors significantly increase an individual’s susceptibility:
- Tobacco Use: Smoking, chewing tobacco, and snuff are major contributors due to the numerous carcinogens present.
- Alcohol Consumption: Heavy and prolonged alcohol use, especially when combined with tobacco, significantly elevates the risk.
- Human Papillomavirus (HPV) Infection: Certain high-risk strains of HPV, particularly HPV-16, are increasingly recognized as a cause of oral precancerous lesions and subsequent cancer, especially in the oropharynx.
- Chronic Irritation: Poorly fitting dentures, sharp teeth, or chronic trauma, though less commonly a direct cause, can sometimes contribute to persistent lesions.
- Ultraviolet (UV) Radiation: Exposure to sunlight is a known risk factor for dysplasia on the lips (actinic cheilitis).
It is important to note that while these factors increase risk, OED can sometimes occur without any clear identifiable cause, underscoring the importance of regular dental check-ups and oral cancer screenings.
Oral Epithelial Dysplasia Treatment Approaches
The primary goal of **oral epithelial dysplasia treatment** is to remove the abnormal tissue and prevent its progression to invasive cancer. The choice of treatment depends on several factors, including the grade of dysplasia, the size and location of the lesion, and the patient’s overall health. Vigilant follow-up and monitoring are essential components of any treatment plan.
Common treatment modalities include:
- Surgical Excision: This is the most common and often preferred method, involving the complete removal of the dysplastic tissue with a margin of healthy tissue. This allows for thorough histopathological examination to confirm the diagnosis and ensure clear margins.
- Laser Ablation: Carbon dioxide (CO2) laser can be used to vaporize or precisely remove dysplastic lesions, particularly for smaller or superficial areas. It offers good precision and reduced bleeding.
- Cryotherapy: This involves freezing the abnormal tissue to destroy the dysplastic cells. It is generally used for smaller, less severe lesions.
- Photodynamic Therapy (PDT): A light-activated drug is applied to the lesion, followed by exposure to a specific wavelength of light, which destroys the abnormal cells. This is a less invasive option for certain cases.
- Close Monitoring and Surveillance: For very mild dysplasia, especially in areas where surgical removal might be complex or disfiguring, a “watch and wait” approach with frequent clinical examinations and biopsies may be considered. However, this requires strict patient compliance and regular follow-up.
Regardless of the chosen treatment, all patients with OED require long-term follow-up due to the risk of recurrence or the development of new dysplastic lesions in other areas of the mouth. This typically involves regular clinical examinations, often every 3-6 months, and repeat biopsies if any suspicious changes are observed. Lifestyle modifications, such as cessation of tobacco and reduction of alcohol consumption, are strongly advised to minimize the risk of recurrence and progression.
