Ollier Disease
Ollier Disease is a rare, non-hereditary skeletal disorder characterized by the development of multiple enchondromas, which are benign cartilaginous tumors that typically affect long bones. This condition primarily impacts bone growth and can lead to skeletal deformities and functional limitations.
Key Takeaways
- Ollier Disease is a rare, non-hereditary bone disorder causing multiple benign cartilage tumors (enchondromas).
- It primarily affects long bones, leading to skeletal deformities and potential limb length discrepancies.
- Symptoms often include bone pain, swelling, and fractures, typically appearing in childhood.
- Diagnosis relies on imaging studies like X-rays, MRI, and sometimes biopsy.
- Treatment focuses on managing symptoms, correcting deformities, and monitoring for malignant transformation.
What is Ollier Disease?
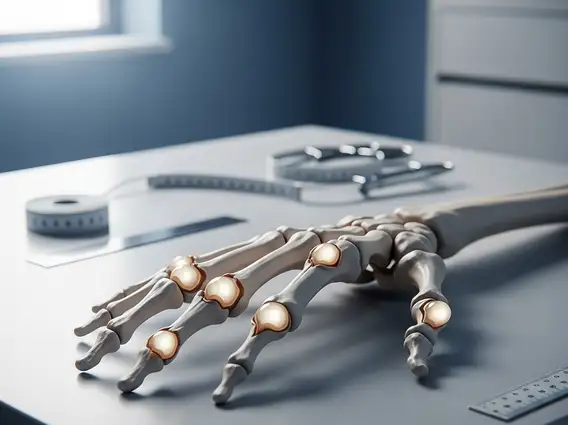
Ollier Disease is a rare, non-hereditary skeletal disorder characterized by the presence of multiple enchondromas, which are benign tumors composed of cartilage that develop within the bones. These lesions typically form in the metaphysis of long bones, such as those in the arms and legs, but can also affect flat bones like the pelvis and shoulder blades. The condition is usually unilateral, meaning it affects one side of the body more severely than the other, though bilateral involvement can occur. It is estimated to affect approximately 1 in 100,000 individuals, making it a very uncommon condition (Source: Orphanet, National Organization for Rare Disorders).
The enchondromas in Ollier Disease arise from remnants of cartilage growth plates that fail to ossify properly. Instead of turning into bone, these cartilage cells continue to proliferate, forming distinct lesions. This abnormal cartilage growth interferes with normal bone development, leading to skeletal deformities, limb length discrepancies, and an increased risk of fractures. The severity and distribution of the enchondromas vary widely among affected individuals.
Ollier Disease Symptoms and Diagnosis
The Ollier disease symptoms typically manifest during childhood, often becoming noticeable when a child is between one and ten years old. The specific symptoms depend on the size, number, and location of the enchondromas. Common manifestations include bone deformities, such as bowing of the limbs, and limb length discrepancies, where one arm or leg is shorter than the other. Patients may also experience bone pain, swelling, and an increased susceptibility to pathological fractures due to weakened bone structure. In some cases, the tumors can be palpable, appearing as hard lumps under the skin.
The Ollier disease diagnosis is primarily based on clinical examination and imaging studies. X-rays are often the first diagnostic tool, revealing characteristic radiolucent (darker) lesions within the bones, indicative of cartilage tumors. Magnetic resonance imaging (MRI) provides more detailed information about the extent and nature of the enchondromas, helping to differentiate them from other bone lesions and assess potential complications. In some instances, a biopsy of the lesion may be performed to confirm the diagnosis and rule out malignancy, especially if there are suspicious features.
- X-rays: Initial imaging to identify characteristic bone lesions.
- MRI: Detailed imaging for lesion extent, nature, and differentiation.
- CT Scans: May be used for complex areas or surgical planning.
- Biopsy: Performed in cases of diagnostic uncertainty or suspected malignant transformation.
Causes and Treatment of Ollier Disease
The exact Ollier disease causes and treatment are complex. While most cases are sporadic, meaning they occur randomly without a family history, genetic research has identified mutations in the IDH1 and IDH2 genes in a significant proportion of individuals with Ollier Disease. These genes play a role in cellular metabolism, and their mutations are thought to contribute to the abnormal cartilage growth seen in the condition. However, the precise mechanisms by which these mutations lead to the development of multiple enchondromas are still under investigation.
Treatment for Ollier Disease is primarily supportive and aims to manage symptoms, correct deformities, and monitor for potential complications. There is no specific cure for the condition. Surgical interventions are often necessary to address limb length discrepancies, correct angular deformities, or remove large, symptomatic enchondromas. Procedures may include osteotomies (bone cutting and realignment), epiphysiodesis (slowing growth in a longer limb), or bone grafting. Regular monitoring with imaging studies is crucial, as there is a recognized risk of malignant transformation of enchondromas into chondrosarcomas, a type of bone cancer, particularly in adulthood. This risk is estimated to be between 10% and 30% over a lifetime.
Patients with Ollier Disease require lifelong follow-up with orthopedic specialists and genetic counselors. Physical therapy can also play a vital role in maintaining joint mobility and muscle strength, improving overall function and quality of life. While some experimental therapies are being explored, they are not standard treatment options. It is important to note that any information on supportive or complementary therapies should be considered as supplementary and does not replace professional medical treatment.