Goiter
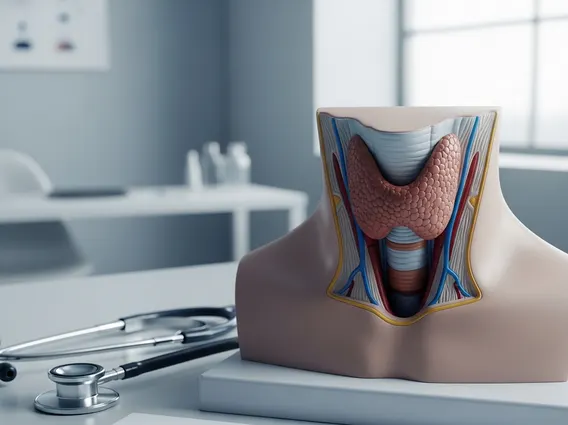
Goiter refers to an abnormal enlargement of the thyroid gland, a butterfly-shaped gland located at the base of the neck. While often harmless, it can sometimes indicate an underlying thyroid condition that requires medical attention.
Key Takeaways
- Goiter is an enlarged thyroid gland, which can be caused by various factors including iodine deficiency and autoimmune diseases.
- Symptoms often include a visible swelling in the neck, and sometimes difficulty swallowing or breathing.
- There are several types of goiter, such as diffuse, nodular, and those associated with hyper- or hypothyroidism.
- Diagnosis involves physical examination, blood tests, and imaging, while treatment ranges from medication to surgery.
- Prevention, particularly for iodine deficiency goiter, often involves ensuring adequate dietary iodine intake.
What is Goiter: Types and Causes
Goiter is the medical term for an enlarged thyroid gland. This enlargement can be diffuse, affecting the entire gland, or nodular, involving one or more distinct lumps within the gland. The thyroid gland is crucial for producing hormones that regulate metabolism, growth, and development.
Understanding goiter types is essential for diagnosis and treatment. Goiters can be classified based on their appearance and function:
- Diffuse Goiter: The entire thyroid gland is enlarged and smooth.
- Nodular Goiter: Characterized by the presence of one or more lumps or nodules within the thyroid gland. These can be single (solitary nodule) or multiple (multinodular goiter).
- Toxic Goiter: Associated with an overactive thyroid gland (hyperthyroidism), leading to excessive hormone production. Graves’ disease is a common cause.
- Non-toxic Goiter: The thyroid gland is enlarged but produces normal amounts of thyroid hormones (euthyroid state). This is often due to iodine deficiency or other factors not directly causing hyper- or hypothyroidism.
The primary causes of goiter are varied. Globally, the most common cause is iodine deficiency, as iodine is essential for thyroid hormone production. According to the World Health Organization (WHO), iodine deficiency remains a significant public health problem in many parts of the world, affecting approximately 2 billion people and being the leading cause of preventable mental retardation. Other causes include:
- Autoimmune diseases: Such as Graves’ disease, which causes hyperthyroidism and diffuse goiter, and Hashimoto’s thyroiditis, which causes hypothyroidism and can lead to goiter.
- Thyroid nodules: Benign or, rarely, malignant growths within the thyroid.
- Thyroiditis: Inflammation of the thyroid gland.
- Certain medications: Such as lithium or amiodarone.
Symptoms and Signs of Goiter
The most noticeable of the symptoms and signs of goiter is a visible swelling at the base of the neck, just below the Adam’s apple. This swelling can range from a small, barely perceptible lump to a large mass that is clearly visible. While many goiters are asymptomatic, larger goiters can exert pressure on surrounding structures in the neck, leading to various symptoms.
Common symptoms include:
- A feeling of tightness in the throat.
- Difficulty swallowing (dysphagia), especially solid foods.
- Difficulty breathing (dyspnea), particularly when lying down.
- Coughing or hoarseness due to pressure on the trachea or recurrent laryngeal nerve.
If the goiter is associated with an overactive thyroid (hyperthyroidism), additional symptoms like weight loss, rapid heartbeat, tremors, and heat intolerance may be present. Conversely, if it’s linked to an underactive thyroid (hypothyroidism), symptoms might include fatigue, weight gain, constipation, and cold intolerance.
Goiter Diagnosis, Treatment, and Prevention
Goiter diagnosis typically begins with a physical examination, where a doctor will feel the neck for thyroid enlargement or nodules. Further diagnostic tests are often required to determine the cause and assess thyroid function. These may include:
| Diagnostic Method | Purpose |
|---|---|
| Blood Tests | Measure levels of thyroid-stimulating hormone (TSH), T3, and T4 to check thyroid function. |
| Ultrasound | Provides images of the thyroid gland, revealing its size, structure, and the presence of nodules. |
| Thyroid Scan | Uses radioactive iodine to assess the gland’s activity and identify “hot” or “cold” nodules. |
| Biopsy | A fine-needle aspiration (FNA) biopsy may be performed to check thyroid nodules for malignancy. |
Goiter treatment options vary widely depending on the underlying cause, the size of the goiter, and whether it’s causing symptoms or thyroid dysfunction. For iodine deficiency, iodine supplements or iodized salt may be prescribed. For hyperthyroidism, anti-thyroid medications, radioactive iodine therapy, or surgery (thyroidectomy) might be considered. Hypothyroidism-related goiters are often treated with thyroid hormone replacement therapy. Small, non-symptomatic goiters with normal thyroid function may only require watchful waiting.
Understanding goiter prevention largely focuses on addressing the most common cause: iodine deficiency. Public health initiatives promoting the use of iodized salt have significantly reduced the incidence of iodine-deficiency goiter worldwide. Regular check-ups can also help in early detection and management of thyroid conditions that might lead to goiter.