Transoral Robotic Surgery
Transoral Robotic Surgery (TORS) represents a significant advancement in the treatment of certain head and neck cancers, offering a minimally invasive approach through the mouth. This technique utilizes robotic technology to enhance precision and improve patient outcomes.
Key Takeaways
- Transoral Robotic Surgery (TORS) is a minimally invasive surgical technique for removing tumors from the mouth and throat.
- The procedure involves a surgeon controlling robotic instruments inserted through the patient’s mouth, avoiding external incisions.
- TORS offers benefits such as reduced pain, shorter hospital stays, and potentially better functional outcomes compared to traditional open surgery.
- Recovery typically involves managing discomfort, dietary adjustments, and speech therapy, with most patients returning to normal activities within weeks.
What is Transoral Robotic Surgery (TORS)?
Transoral Robotic Surgery (TORS) is a sophisticated, minimally invasive surgical technique used primarily to remove tumors from hard-to-reach areas of the mouth and throat, including the tonsils, base of the tongue, and larynx. This approach allows surgeons to access these areas through the patient’s mouth, eliminating the need for large external incisions that are often associated with traditional open surgeries. By utilizing advanced robotic systems, TORS provides surgeons with enhanced visualization, dexterity, and precision, which are crucial for operating in confined spaces.
The development of TORS has revolutionized the treatment landscape for certain head and neck cancers, offering a less invasive alternative that aims to preserve critical functions such as speech and swallowing. It is typically employed for early to moderately advanced cancers, often reducing the need for extensive radiation or chemotherapy post-surgery, or allowing for a more targeted approach when these therapies are still necessary.
The Transoral Robotic Surgery Procedure
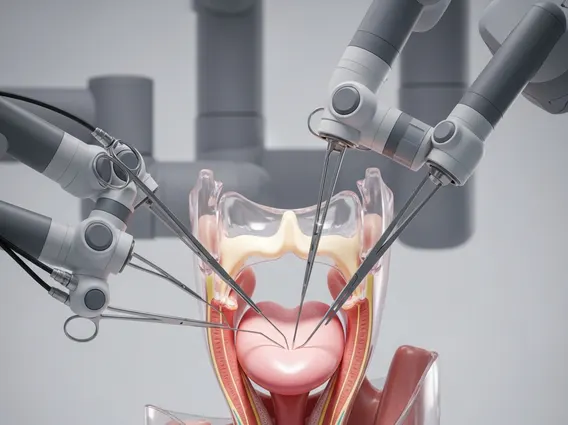
The transoral robotic surgery procedure involves a highly skilled surgical team, including the surgeon, anesthesiologist, and nurses. During the procedure, the patient is under general anesthesia. The surgeon sits at a console, controlling robotic arms that are equipped with specialized surgical instruments and a high-definition 3D camera. These instruments are carefully inserted through the patient’s mouth to reach the tumor site.
The robotic system provides the surgeon with a magnified, three-dimensional view of the surgical field, allowing for precise identification and removal of cancerous tissue while minimizing damage to surrounding healthy structures. The robotic instruments have a greater range of motion than the human wrist, enabling intricate dissections in tight anatomical spaces. Once the tumor is removed, the instruments are withdrawn, and no external stitches are typically required. The procedure’s duration varies depending on the size and location of the tumor.
Key steps in the procedure often include:
- Patient positioning and general anesthesia.
- Insertion of a mouth retractor to provide access to the surgical site.
- Docking of the robotic system, with instruments and camera carefully guided into the oral cavity.
- Surgeon controls robotic arms from a console, performing tumor resection with enhanced precision.
- Removal of the resected tissue and instruments.
Benefits and Recovery from Transoral Robotic Surgery
The benefits of Transoral Robotic Surgery are numerous, particularly when compared to traditional open surgical techniques. Patients often experience less pain, reduced blood loss, and a shorter hospital stay. The minimally invasive nature of TORS also leads to smaller scars (or no visible scars at all), and a quicker return to normal activities. Furthermore, TORS can result in improved functional outcomes, such as better preservation of speech and swallowing functions, which are critical for quality of life after head and neck cancer treatment.
Transoral robotic surgery recovery typically involves a period of healing and rehabilitation. Immediately after surgery, patients may experience a sore throat, difficulty swallowing, and some discomfort, which can be managed with medication. A temporary feeding tube might be necessary for some patients if swallowing is severely affected, though many can transition to a soft diet relatively quickly. The length of hospital stay is generally shorter, often just a few days. Rehabilitation, including speech and swallowing therapy, is often initiated soon after surgery to help patients regain full function. Most patients can expect to return to their normal daily routines within a few weeks, though full recovery of speech and swallowing may take longer, varying by individual and extent of surgery. According to the National Cancer Institute, minimally invasive approaches like TORS can lead to fewer complications and faster recovery times compared to open surgery for certain head and neck cancers.