Pelvic Lymphadenectomy
Pelvic lymphadenectomy is a surgical procedure involving the removal of lymph nodes from the pelvis. This intervention is crucial in the diagnosis and staging of various cancers, particularly those affecting the pelvic region, to assess disease spread.
Key Takeaways
- Pelvic lymphadenectomy is a surgical procedure to remove lymph nodes from the pelvic area.
- It is primarily performed to diagnose and stage cancers, such as prostate, bladder, cervical, and endometrial cancers.
- The procedure helps determine if cancer has spread to the lymph nodes, guiding further treatment decisions.
- It can be performed via open surgery or minimally invasive techniques like laparoscopy or robotics.
- Potential risks include bleeding, infection, nerve damage, and lymphedema.
What is Pelvic Lymphadenectomy?
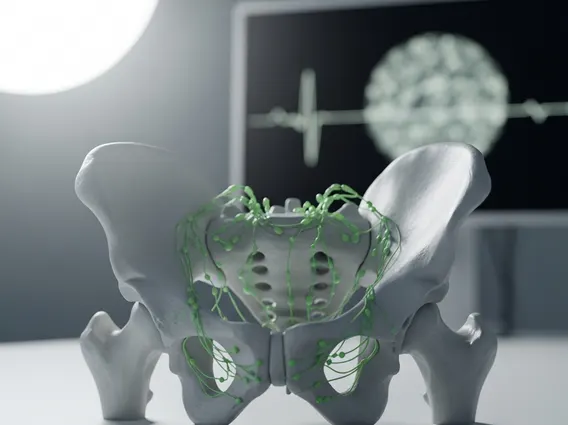
Pelvic lymphadenectomy refers to a surgical procedure where lymph nodes are removed from the pelvic region. These lymph nodes are an integral part of the lymphatic system, a vital component of the body’s immune defense responsible for filtering waste and housing immune cells. The primary goal of this procedure is to examine these nodes for the presence of cancer cells, which helps in determining the extent of the disease and guiding subsequent treatment strategies. This surgical intervention is crucial for accurate cancer staging and prognosis.
The procedure involves carefully dissecting and removing specific groups of lymph nodes within the pelvis, depending on the type and location of the primary cancer. For instance, in prostate cancer, obturator and external iliac nodes are often targeted, while in gynecological cancers, a broader range of pelvic nodes might be removed. The removed tissue is then sent to a pathologist for microscopic examination to detect any metastatic cancer cells. This detailed analysis provides essential pelvic lymph node dissection information that informs oncologists about the cancer’s aggressiveness and spread.
Reasons for Pelvic Lymph Node Dissection
There are several compelling reasons for pelvic lymphadenectomy surgery, primarily centered around cancer diagnosis, staging, and sometimes, treatment. The most common indication is to determine if cancer has spread from its primary site to the regional lymph nodes. This information is critical because the presence of cancer cells in lymph nodes often indicates a more advanced stage of the disease, necessitating more aggressive treatment.
Common cancers for which pelvic lymphadenectomy is performed include:
- Prostate cancer
- Bladder cancer
- Cervical cancer
- Endometrial cancer
- Ovarian cancer
- Rectal cancer
According to the American Cancer Society, lymph node involvement is a significant prognostic factor for many of these cancers, influencing treatment choices such as chemotherapy, radiation therapy, or further surgery. For example, in early-stage cervical cancer, a pelvic lymphadenectomy can help identify microscopic spread, which might not be detectable through imaging alone, thereby preventing undertreatment. In some cases, removing affected lymph nodes can also serve a therapeutic purpose, reducing the overall tumor burden.
The Pelvic Lymphadenectomy Procedure Explained
The pelvic lymphadenectomy procedure explained involves several key steps, typically performed under general anesthesia. The approach can vary significantly, ranging from traditional open surgery to minimally invasive techniques such as laparoscopy or robotic-assisted surgery. The choice of technique depends on factors like the patient’s overall health, the extent of the cancer, and the surgeon’s expertise.
In an open procedure, a single, larger incision is made in the lower abdomen to access the pelvic cavity and remove the lymph nodes. Minimally invasive approaches, conversely, involve several small incisions through which a camera and specialized surgical instruments are inserted. Robotic-assisted surgery, a type of laparoscopy, provides the surgeon with enhanced dexterity and 3D visualization. Regardless of the technique, the surgeon carefully identifies and removes the targeted lymph nodes, ensuring surrounding vital structures like nerves and blood vessels are preserved. The removed nodes are then sent for immediate or delayed pathological analysis. Post-procedure, patients are monitored for recovery, with hospital stays varying based on the surgical approach and individual patient factors. Recovery typically involves managing pain, monitoring for complications, and gradually resuming normal activities.
